PBHL20009 Assessment 2 Sample
Question:
Your essay must consist of your reflection on the evolving situation that has taken place during the course of term 2 2020 and term 1 2021. The focus of the essay is to show your deepening understanding of issues that may arise during a public health event, especially as they relate to cross-cultural communities like the one we live in, and yourself as a developing practitioner. Your essay should address the following points:
1) A very brief summary of the current pandemic and its effects in the place where you live
2) The actual effects on our cross-cultural community
3) The potential effects of this kind of situation on a cross-cultural community
4) What have you, as a developing public health practitioner learned from experiencing a real-life public health emergency.
Answer:
In recent times COVID 19 pandemics caused by coronavirus which has spread from China and very new to the world and affected the world population drastically. The COVID 19 pandemic impacted on Australia and especially on the population of Sydney. I can see that the economic, social and political situations are very much affected by the virus spread as the contamination of the virus is uncontrollable and higher level of contamination developed a certain amount of panic among people as well. As a developing public health practitioner, I can also experience the psychological impacts among people due to the change in the social processes and rising unemployment issues along with an instable economic situation. I have seen that the COVID 19 pandemic developed several issues and the only way to reduce the impact of the virus was global lockdown and rapid vaccination to build immunity against the virus. However, the virus shown a characteristic of changing its functionality and structure and thus, there are different species have been found till now from the end of 2019 when the virus outbreak occurred from China. Considering all these factors, I have seen that the Australian government and local government of NSW developed the regulation of lockdown especially marking some hotspots where the rate of COVID cases is high (NSW Government, 2021). Sydney have several hotspots, though, due to 80 per cent of population of Sydney have been administered with first dose of vaccine till 20 th September 2021 and the curfew or strict lockdown of the 12 hotspots of Sydney has been lifted (The Guardian 2021). However, as per my knowledge, regulation developed by the government highlighted that if there is any single new case can be found among these areas the lockdown will again be put forward for at least 14 days (The Guardian 2021). As a developing public health practitioner, I think in this dire situation this is the only solution for the people to be safe and reduce the contamination of corona virus.
I can state that the situation of COVID 19 cannot be marked as positive even after almost one and half year of the pandemic impact on the world population. As a developing public health practitioner, I can state that the impact of the pandemic is still present and the regulation of NSW government is strict to improve the situation (NSW Government 2021). The regulations include travelling outside the local area without proper permission and identification of the contamination free situation for any individual which can be visible to me and others still now as in Sydney a truck driver found with the infection and a 31-year-old woman travelling outside the area has been confronted by the police as well (Abc.net.au 2021). Considering all these factors, I can highlight that the regulation of the lockdown and curfew are still implemented by the government for the safety of the local and national population. However, there are 628 cases including 3 deaths due to COVID 19 found in the area of Victoria and the government put forward the regulation regarding vaccination of education staffs till November to continue the educational works as well (Abc.net.au 2021). Hence, as a developing public health practitioner, I can reflect that the policies and regulations can be effective.
However, I think that the empowerment to the people will help them to understand the importance of the policies and regulations. Thus, as per my experience and knowledge I reflect that the empowerment programs for people should be considered with higher priority. However, the requirement of the hand washing, face mask and face shield usage related education to people cannot be neglected and I should try to educate andempower people regarding the use of these factors. I think that the vaccination can provide immunity though developing habit of healthy practices is necessary to reduce the risk of the COVID 19 pandemic. Considering this, I can highlight that hand washing is done through 7 steps as per regulation of WHO and these should be considered to improve the health education of people and also the proper face mask wearing processes should be considered as well for the empowerment process (Who.int, 2021). Moreover, the regular sanitisation is also required to be considered for the safety from the virus and I should also practice that and influence people to do so as well.
People from various cultural backgrounds are being influenced differently by the epidemic. SBS, a multi-ethnic and multilingual broadcaster, claimed that people were being misled by alleged therapies that had no proven impact, such as utilising salt water, garlic, vitamins, and whiskey as home cures. Others were said to be utilising traditional remedies, and certain religious groups were led to think that fervent religiosity would provide them with viral protection. They felt they could disregard government public health recommendations and legislation (SBS, 2020). SBS said that public education initiatives in languages other than English were minimal and ineffective. Better, culturally relevant information, for example, would enhance public messages on
hygiene and physical distance (SBS 2020). COVID-19 also resulted in a rise in racist complaints to the Human Rights Commission. Since the beginning of February, one-third of all complaints have been linked to the virus. These included reports of verbal and physical assault, as well as vandalism (Human Rights Commission 2020), with Chinese individuals being particularly targeted and, as a result, suffering from insecurity, fear, and mental illness (Fang and Yang 2020).
I can also necessarily highlight that the supplies of medication and other products are also delayed due to the lockdown and the imbalanced international situation. Hence, I can reflect that the change in the situation is not possible at this moment properly as the global pandemic situation is not normalised yet. Moreover, as a developing public health practitioner, I can see that the social and psychological situation of people is also not in a proper shape. Hence, I should consider empowerment and educational programs for the people to reduce the impact of the pandemic situation and promoting wellbeing for them. However, the unemployment and the social distancing affected on the economic and psychosocial aspects of people in a drastic manner. Considering all these factors, I can highlight that the importance of the normalisation of the situation through proper strategic implementation should be considered by the government. Though, the impact of the international economic situation and the employment situation are not positive. Hence, based on all these situational contexts of the local area of Sydney and also the national and international context, it is evident that the health care is hampered due to the social determinants of health are impacted drastically.
Moreover, the overwhelming cases of COVID 19 lead to the imbalance in the work force and work load. Other than all these, the lockdown regulations impacted negatively on the supply of medical products as well (van Barneveld et al. 2020).I can state that the impact of COVID 19 on health care department is very much prominent due to the sudden change in the care regulations and demands as well. However, I think that the social and political along with the economic factors that have been adversely affected due to the pandemic developed the negative situation in a more prominent manner. I also realise that the lockdown regulation led to a gap in the social interactions and also impacted on the psychological aspects of people (van Barneveld et al. 2020). Hence, the health care department should be focused on the planning for the effective care delivery to these people as well and I should take part in the proper care delivery planning. Moreover, the technological use of the social media based or the telephonic care delivery processes should be prioritised for the improvement of the situation and also the cost and time reduction for care delivery. The COVID pandemic is going to be tougher in few months as well as the 3 rd wave or the Delta strain of COVID 19 will infect as per the health scientists. Thus, I think it is necessary to state that the consideration of the change in the health care work force or processes should be prioritised for the improved care delivery to the COVID patients as well as the people affected with other comorbidities to maintain the quality of care. The regulations should be strictly followed and it can provide a better situation to cope with the adverse impact of the disease. The prospect of almost 2 years of prolonged impact of a virus on human health in a drastic manner is very much rare situation for health care department (Bateson et al. 2020). Hence, I think that in this sudden and drastic issue the health care department is trying to cope and it can be stated that the international situation impacts more adversely and delays the improvement against the disease or virus.
It is evident to me that with proper infrastructure and work force the health care department can reduce the impact of the disease in a positive manner. The general impacts in the Sydney and Australian contexts are also impacted with the issues of the cross-cultural communities and also the people from other minority groups. It has been seen that the cross-cultural group of people and also the minority people have barriers of language and also cultural differences (Spennemann 2021). As a developing public health practitioner, I think that the linguistic barrier develops gap in the care access and also reduce the chances of proper interaction with the health care professionals or the majority of the population (OECD 2020). Hence, I can reflect that there is a social gap develops which is prominent and negatively impact on the health outcome of these people. Based on this context, I can necessarily highlight that the language-based issues should be reduced through the implementation of the positive communication strategies. The nurses and other health care workers should show empathy and use the non-verbal communication strategies to communicate with these people. I think that as a developing public health practitioner, and other health care professionals along with the people can access the health care appropriately.
The cross-cultural people and also the minority people showed different cultural beliefs and actions in different situations. I can also reflect that the impact of these activities lead to different issues in several situations. Thus, it is necessary to provide proper care and empowerment to these people to follow the regulations of COVID 19 and reduce the impact of the disease on them. In this manner, the situation will be improved and the reduction of the negative consequences can be achieved. The factor of the change also depends on the attitude of the health care workers (OECD 2020). It has been seen that the cross-cultural people are neglected and discriminated by the White population in several cases and it also develops unnecessary communication
gaps and impacts on the health care process. Thus, the consideration of the change in the situation through the empowerment of the health care workers should also be considered for the improvement in the care process (Cui et al. 2021). Thus, as a developing public health practitioner, I can necessarily highlight that the self- actualisation of people is very much important considering the national, local and also international situations of COVID 19. Though, the health care workers should reduce the attitude of discrimination and provide culturally safe and collaborative care to each and every patient needing health related support.
As a health care worker, the COVID 19 pandemic is one of the crucial issues I have faced in my entire career and maintaining the safety of the co-workers, patients and myself should be considered by me at the first place. The aspect of the care delivery and also considering the priorities and needs of the patients are very much important for me. However, in terms of the experience in Sydney as a nursing care professional I understood my duties and the impacts of life threats as well. The COVID 19 pandemic developed a panic among the health care workers as well as among the patients (Bateson et al. 2020). I should also state that I have found that the impact of the cultural differences of people should not affect the care delivery process or health outcome of the patients. Hence, I should promote cultural safety and provide equal care to all the patients. Moreover, I should focus on empowering people regarding the DOs and DON’Ts to avoid the risk of the COVID 19 or other comorbidities of the disease. However, the recent data of the Sydney and other areas of NSW developed a concern and I should focus on helping people to improve their own situation regarding the health outcomes along with the community people as well. The cultural safety should be considered with priority by me as well.
References
Abc.net.au, 2021, ‘Truck driver 'presumed' to have Delta was in WA for two days — as it
happened’, viewed 29 September 2021 <https://www.abc.net.au/news/2021-09-22/covid-updates-sydney-melbourne-cases-restrictions-border/100481082>
Bateson, D, Lohr, P, Norman, W, Moreau, C, Gemzell-Danielsson, K, Blumenthal, P, Hoggart, L, Li, H, Aiken, A & Black, K, 2020, ‘The impact of COVID-19 on contraception and abortion care policy and practice: experiences from selected countries’, BMJ Sexual & Reproductive Health, vol. 46, no. 4, pp.241-243, viewed 26 September < https://srh.bmj.com/content/familyplanning/46/4/241.full.pdf>
Cui, J., Mao, L., Newman, C., Kwan, C. and Lancaster, K., 2020. ‘Managing Risk in the Pro-Empowerment Era of Mental Health Care: A Cross-Cultural Study of Social Work Perspectives in Hong Kong and Sydney’. The British Journal of Social Work, 51(3), pp.831-848, viewed 29 September 2021 < https://academic.oup.com/bjsw/article-abstract/51/3/831/6044335>
Fang, J., Yang, S. (2020). ‘Chinese-Australian family targeted over coronavirus receives outpouring of support, ABC’, viewed 29 September 2021 <https://www.abc.net.au/news/2020-04-23/chinese-australian-family-racist-coronavirus-racist-attack-speak/12178884>
Health.gov.au, 2021. ‘COVID-19 Vaccine Roll-out Jurisdictions Breakdowns.’, viewed 29 September 2021 <https://www.health.gov.au/sites/default/files/documents/2021/09/covid-19-vaccine-rollout-update jurisdictional-breakdown-29-september-2021.pdf>
Human Rights Commission. (2020). ‘Where’s all the data on COVID-19 racism?’,
viewed 29 September 2021 < https://humanrights.gov.au/about/news/opinions/wheres-all-data-covid-19-racism>
NSW Government, 2021. ‘Greater Sydney restrictions.’, NSW Government, viewed 29 September 2021 <https://www.nsw.gov.au/covid-19/rules/greater-sydney>
OECD, 2020. ‘Culture shock: COVID-19 and the cultural and creative sectors.’, OECD. viewed 29 September 2021 <https://www.oecd.org/coronavirus/policy-responses/culture-shock-covid-19-and-the-cultural-and-creative-sectors-08da9e0e/>
SBS Australia. (2020). ‘Harmful coronavirus myths are being spread in Australia’s multicultural communities.’, viewed 29 September 2021 <https://www.sbs.com.au/news/harmful-coronavirus-myths-are-being-spread-in-
australia-s-multicultural-communities>
Spennemann, D., 2021. ‘No Entry into New South Wales: COVID-19 and the Historic and Contemporary Trajectories of the Effects of Border Closures on an Australian Cross-Border Community.’, Land, 10(6), p.610, viewed 29 September 2021 & lt;https://www.mdpi.com/2073-445X/10/6/610/pdf>
The Guardian, 2021. ‘New NSW Covid lockdown restrictions: update to Sydney, regional NSW and Canberra, ACT coronavirus rules explained.’, viewed 29 September 2021 <https://www.theguardian.com/australia-news/2021/sep/22/new-nsw-covid-lockdown-restrictions-update-to-sydney-regional-nsw-and-canberra-act-coronavirus-rules-explained>
van Barneveld, K., Quinlan, M., Kriesler, P., Junor, A., Baum, F., Chowdhury, A.,Junankar, P., Clibborn, S., Flanagan, F., Wright, C., Friel, S., Halevi, J. and Rainnie, A.,2020. ‘The COVID-19 pandemic: Lessons on building more equal and sustainable societies.’, The Economic and Labour Relations Review, 31(2), pp.133-157, viewed 29 September 2021 <https://journals.sagepub.com/doi/pdf/10.1177/1035304620927107>
Who.int, 2021. Coronavirus disease (COVID-19): Masks. [online] Who.int., viewed 7 October 2021 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-masks Who.int, 2021. Hand Hygiene: Why, How & When?. [online] Who.int., viewed 7 October
2021
https://www.who.int/gpsc/5may/Hand_Hygiene_Why_How_and_When_Brochure.pdf
Who.int, 2021. World Hand Hygiene Day 2021: Seconds save lives - clean your hands!.[online] Who.int., viewed 7 October 2021 https://www.who.int/campaigns/world-hand-hygiene-day/2021
PUBH6001 Health Policy and Advocacy Assignment Sample
Assignment Brief
Individual/Group - Individual
Length - 2000 words (+/?) 10%)
Learning Outcomes
This assessment addresses the following learning outcomes:
Analyze different theories and approaches to policy agenda setting
Apply knowledge of policy development to a public health policy issue
Analyze issues in contemporary Australian health care policy
Develop processes for the evaluation of and accountability for policy
Critique the role of networks and coalitions in the policy agenda setting process
Submission - Sunday of week 8 at 11.55pm*
Weighting - 40%
Total Marks - 100 marks
Instructions:
In this Assessment, you will engage in policy analysis. For assignment help Choose a health policy (either current or past), either at the state or federal level, to analyses in this Assignment (e.g., mental health policy, women’s health policy, preventative health policy, men’s health policy, Aboriginal and Torres Strait Islander health policy). The Assignment should be approximately 2,000 words (+/? 10%) and presented in essay form. Address the following questions in your Assessment but please do not answer the questions as a series of short answers:
Firstly, provide a short introduction to your essay. Then proceed to analyses your chosen policy, and in doing so, consider the following issues:
The Problem and Context
• Describe the current and historical policy context of the problem.
• What is the problem which the policy seeks to address?
• What problems are highlighted?
• What problems have been overlooked?
Frame of Reference/Dominant Discourse
•What is the common frame of reference or dominant discourse evidence within this policy???
•Are certain words and phrases commonly used?
•Are there any underlying assumptions behind these?
Targets, Stakeholders and their Representation
•Who is the target of the policy (the subject of the discourse)?
•Who are the other stakeholders identified in the policy? Describe key institutional structures, agencies and workforce capacity building.
•How are the subjects of the policy being represented?
•How are different social groups portrayed in this policy and what implications does this have?
•Are there any moral judgements expressed in this representation?
Policy process
•Who were the stakeholders involved in the development of the policy? Who was overlooked?
•Whose interests were represented in the development of the policy? Which voices were not heard?
•What were the potential competing interests and power differentials of those involved in the development of the policy?
•What was the motivation for stakeholders in creating this policy?
•Were there any particular windows of opportunity that enabled the development of this policy?
Policy Solutions
•What solutions are put forward to address the problems?
What alternative solutions might have been overlooked?
•Are there any social/power/ethical implications of this policy?
Effectiveness
•Consider the implementation of the policy. How effectively do you think the current policy has been implemented?
•What are the accountability processes for the policy?
•Consider evaluation measures (indicators) and any evaluation which has been undertaken.
•How effective has the policy proven to be?
Finally, finish your essay with a conclusion.
Assessment Criteria:
• Knowledge and understanding of the policy issue (30%)
• Critical analysis of the problem, frames of reference used, the policy process and policy solutions (30%)
• Application and synthesis of knowledge about policy theories (25%)
• General Assessment Criteria (15%) Assessment fulfills general academic standards, including: Provide an introduction and conclusion
• Complies with academic standards of writing, including legibility, clarity, accurate spelling, presentation and grammar.
• Uses appropriate APA 6 style for citing and referencing research
• Upholds standards of academic integrity, as demonstrated by acceptable report from text?matching software (e.g. Safe Assign).
Solution
Women’s health policy
Introduction
Australia was among the first countries to adopt a health and wellness related strategies specifically for women. The National Women’s health Policy was embraced to strengthen and to enhance the health and well-being of every Women and girls living in Australia, especially those who are more susceptible to poor health. The National Women’s health Policy 2010 was created on the concrete foundation of the first National Women’s Health Policy: Advancing Women’s health in Australia. The National Women’s health Policy now helps to address the challenges faced by Women in sustaining good health in the 21st century. There has been a serious rise in diseases affecting women today. But, unfortunately, there are major inequalities in the wellness status of several Australian women (Dc.cod.edu, 2021). The woman from lower socio-economic groups, Aboriginal background and Torres Strait Islanders still face hardships regarding health care. The aim of the new and improved health care policies for Women strives to enhance the health care conditions of all women, especially those prone to poor health. Based on the National Women’s health Policy 2010, the National Women’s health Strategy for 2020 to 2030 was adopted for even more improved health care for Women (Nakray, 2013). This report shall dive deeper and find out more detailed information about Women’s health care polices of Australia.
The problem and Context
Women’s health has been neglected in the society for long. It was time that women are treated as equal subjects in the society whose health needs must be catered to. Thus, the policy makers felt the need for framing policies that would help in the upliftment and improvement in the health of women in the country. The window of opportunity when the framing and implementation of the women health policy is the fact that it will help in improving the health index of the country which will consequently help in enabling growth and development in the country.
The 1stNational Women’s health Policy of Australia was adopted in the year 1985. In the Adelaide conference (September of 1985), more than 700 Women together produced a bipartisan agreement stating that the National Women’s health Policy, should be focus on Women ’s position in the society, how it affects the status of their health and accessibility in wellness treatment facilities.
In order to create the Women’s health policy, an extensive consultation process was followed yearning to discuss the ‘Women’s health: a framework for change‘. Meetings were held across all capitals cities and few handpicked villages, 300+ written documents were submitted, which clearly conveyed the message to the government to know the real situation and how it impacted the lives of the women in the country. The Women of Australia contributed a huge deal in the development of the First National Women’s Health Policy.
The problem prioritised in the 1989 policy were Health of aging Women, Reproductive health and sexual health, Personal and mental health, Livelihood Health and Safety, Violence against Women, Women’s health as care givers and the impact of prejudice against women on Women’s health. Some strategies also recognized five field regarding Women’s concern about structure of health care and information –Outlay of health services for Women, provide with health related information, collection of data as well as research, participation of Women in making decisions in health sector, equipping health care providers A majority of health problems were established with the aid of study and analysis, which represent the significant problems related to mortality and diseases among women in the next twenty years.
Firstly, the health focus area is preventing severe illness by controlling the danger, targeting severe illness like diabetes, cardiovascular illness, and cancer. And also by preventing risk factors like nutrition, obesity, drug consumption, inactivity in life style, alcoholism. The policy encourages getting a detailed insight of Women’s lives, containing the obstacles that prevent Women adopting healthy lifestyles and behaviours. Secondly, the focus area is taking care of the mental state and health, depression, targeting anxiety, and suicide for women. Thirdly, the focus area is reproductive and sexual health; providing information and educating people on sexual health, safe coitus practices, reproductive health, and maternal health. Maintaining a healthy lifestyle and staying fit before, during and in the postpartum period may have a significant and long-term impact on both the mother's and the kid 's health. And finally, good ageing focuses on illnesses such as musculoskeletal injuries, dementia, and disability. The strategy emphasises that the economic, cultural, and environmental conditions in which women reside and age can have an effect on their later years. However, despite the policies and strategies that have been implemented by the government of Australia in context to women’s health, not much improvement has been seen in the overall health of the women of Australia. This is probably because of the lack of a procedural means to implement the policies and strategies of women health as a result of which desired outcome is not attained.
Frame of Reference/Dominant Disclosure
There has been significant improvement in Women’s wellness care since the introduction of Women’s health treatment strategies. However, these improvements are not equally achieved throughout Australia. Women from certain group like the Aboriginal and Torres Strait Islanders involvement much worse health. Even though some agenda of the National Women’s health Policy 2010 has initiatives to eradicate inequality in health care, there are little evidence of how much it has been able to achieve success in real situations of those Women (Phaa.net.au, 2021).
There is a severe lack in fund for these policies, which is not highlighted like its principles are. Apart from that some Australian Women feel that NWHP and NWH Program only address the interests of Anglo-Australian women from middle class background (Awhn, 2021). The problems of the Aboriginal Women were however left out as discussed earlier. The National Aboriginal Health Strategy, was adopted to deal with Aboriginal Women’s health. But regrettably, it was never funded sufficiently. An evaluation in the year 1994 brought to light -gross under-funding by all governments, absence of accountability, absence of political support for the National Council of Aboriginal Health that was created to supervise implementation.
No satisfactory long term outcome was achieved even after positioning immigrant and refugee women differently. The National Non-English Speaking Background Women’s health Strategy (NESBWHS) was created to help these women.
Keywords like Women, Aboriginal Women, National Women’s health Policy, strategy, health, health issues can be seen throughout. It is assumed that the National Women’s health Policy and other programs are enough for resolving all issues and problems related to Women but in reality they fall short to cover the entire aspect of Women’s health.
Targets, Stakeholders and their representation
The main target of the National Women’s health Policy, National Women’s health Strategy, National Non-English Speaking Background Women’s health Strategy (NESBWHS), etc. is Women of Australia (Dalinjong & Homer, 2018). All these policies are targeted towards improving Women’s health. Australia launched the National Women’s health Policy in 1989 and became the only country to have a comprehensive policy on Women’s health care. The policies are meant to deliver conventional and diverse Women’s health services. The other stakeholders of the women health policy include the healthcare professionals including doctors and nurses as well as the government as they play an important role in improving the overall health of women in the country. They also have a very big role and representation to play in the implementation of the women health policy aimed at improving the overall health of the women of the country. Both the government as well as non-governmental organizations ensure that the health needs of the women in Australia are catered to. They constantly monitor the policy and the impact that it has on the overall health of women in the country.
The idea of Women as central principal of the policy was widely supported. One of the main principles of the policy was equality among women regarding health care. Because of the high risk that the Torres Strait Islander Women and Aboriginal Women faced in poor health, they were oftentimes prioritised (Vasilevska & Fisman, 2012). The other groups of Women who were at high risk of inferior health were- Women with disability, Women who are caregiver, Women living in remote areas or rural areas, refugee Women, migrant Women, Elderly Women, and bisexual and lesbian Women. Active participation of the different groups of Women in designing the policy, implementing the strategies which affect them, helping to facilitate that the health aids and information are designed keeping in mind the needs of people who require it the most (Awhn.org.au, 2021). The participation of women in making these policies strongly suggests involving expert opinion of women from various communities in implementation of the local programs which aim to improve the health of women in the country.
Policy Process
The National Women’s health Policy is a unique proposition specifically designed for women and girls in Australia. The policy was created specially with women prone to poor health in mind. The 1989 policy was designed to solve the problem related to Women’s health of that era (Wohler & Dantas, 2017).
Over the past decades, the 1989 policy for women’s health has been the footing for expansion of new programs for women’s health. A majority of health care establishments were built or renovated; health care providers were trained in a new and integrated way. Australian Longitudinal Study on women’s health was established because of 1989 policy.
The National Women’s health Policy was developed on the basis of 1989 policy. This policy had a dual approach addressing immediate and future health challenges of Women. It equally prioritised- Administration and advancement of health care facilities and preventive strategies to care and prevent through targeted health issues that will have a massive effect on the following twenty years and dealing with the social determinants of health in order to curb health inequalities.
Policy Solutions
The government of Australia is based on improving and motivating decent wellness of everyone and supports obstructive efforts which may help to address particular health problems raised by Women through this policy.
Chronic diseases are one of the biggest health issue faced in Australia, which causes death, disability and sickness among the population. But chronic diseases can be reduced by prevention, modifications of lifestyle and providing support. The Australian Government has taken numerous initiatives to help prevent and manage chronic diseases, one such example is the Australian Chronic Disease Prevention Alliance. Over the past decade, ACDPA has operated with the government, stakeholders and public health groups to boost nutrition, increase physical activity and reduce obesity among the population.
Mental health conditions can be a silent killer. In today’s world mental health issues are rapidly increasing and affecting huge masses of the population all around the world (Hajizadeh & Butler, 2014). Women are more prone to experience mental health problems from various issues like domestic violence, family pressure, post partum depression etc. The Australian Government has taken multiple initiatives to help prevent and cure mental illnesses. Some of them are The National Mental Health Policy of 2008, beyond blue: The National Depression Initiative, Forth National Mental Health Strategy and headspace
Most deadly and dangerous sexually transmitted diseases can be prevented very easily. The Australia’s Health Ministers Committee (AHMC) promoted the New National Strategy for prevention of STIs, BBVs, and HIV.
The Australian health ministry has taken several initiatives to help mothers before, during and after child birth. Initiatives like- the Australian National Breastfeeding Strategy 2010–2015, National Maternity Services Plan, et al to support mothers and reduce mortality rate in new-borns. Apart from this, the government must also employ volunteers who shall spread awareness regarding women health, this will help in educating people on serious issues like women’s health. The social implication of these policies implemented by the regulatory bodies is reflected by the importance that the government bestows on the health of women. This empowers women who feel important and cared. Apart from this, this is the ethical thing to do as women have been neglected in the society at large and now, it is time to give them equal importance as the men of the society.
Effectiveness
Australia launched the first National Women’s health Policy in 1989 and since then Women have experienced significant economic, social and technological changes. Based on the policy of 1989, the National Women’s health Policy 2010 and the National Women’s health Strategy 2020 to 2030 has been created to make improvements in women health policy. The overall health of women in the country has witnessed considerable improvement over time (ray Jamieson, 2012). Diseases like cardiovascular disease, cancer, smoking rate in women have noticed a declining trend.
On one hand it can be said that the women’s health care policies have changed the National health policy to a great extent. We now have a modified and integrated women’s health policy that is inclusive of the arguments made by feminist like a national plan to combat violence against Women and the National Disability Strategy that meets the ethical needs and engages a sex inequality (Long& Baer, 2018). While on the other hand much of the changes clearly reflect a substantive political action. Health care for Women or anyone else, at the decision making help is still limited to primary health care and hospital levels, as the investments made for it is very small. The accountability of the success or failure of the policy lies in the hands of the policy makers who frame and implement the policies aimed at improving the health of women in Australia. The improving overall health of women as reflected by the statistical data is an evidence of the effectiveness of the women health policies and strategies implemented by Australia.
Conclusion
The National Women’s health Policy of 1989 was a remarkable mile stone that set the tone for future developments of health care specially tailored to fit the needs of women. In all, the government has taken great initiatives, and helped prioritize and endorse Women’s health care system. The Australian government has formulated lots of collection of policies, strategies, initiatives, programs and plans to health. The NWHP was the first of its kind health policy specially designed for women which inspired many such models across the world (Awhn, 2021).
The separation of women’s health sector has resulted in a plethora of successful achievements. Differentiation of access to health care of Aboriginal, Torres Strait Islanders, Women with disabilities, has considerably lowered.
With improved health care the quality of life of Australian Women has improved considerably (health.gov.au, 2021). Thus it can be concluded that the National Women’s health Policy has proven be a great achievement and has considerably been able to enhance wellness protection requirement of Australian Women, specifically the Aboriginal and Torres Strait Islander Women
References
Awhn.org.au. (2021). Retrieved 24 March 2021, from http://awhn.org.au/wp-content/uploads/2015/03/38_NationalWomensHealthPolicysummary.pdf
Dalinjong, P. A., Wang, A. Y., & Homer, C. S. E. (2018). Has the free maternal health policy eliminated out of pocket payments for maternal health services? views of women, health providers and insurance managers in northern Ghana. Plos One, 13(2), 0184830.
Dc.cod.edu, (2021). [online] Dc.cod.edu. Retrieved 24 March 2021, from https://dc.cod.edu/cgi/viewcontent.cgi?article=1630&context=essai
Hajizadeh, M., Connelly, L. B., & Butler, J. R. G. (2014). Health policy and equity of health care financing in Australia: 1973-2010. Review of Income and Wealth, 60(2), 298–322
health.gov.au. (2021). Department of Health | Women's Health. Retrieved 24 March 2021, from https://www1.health.gov.au/internet/main/publishing.nsf/Content/national%20womens%20health-1
Long, D., & Baer, H. (2018). Health anthropology in australia: special section on medical anthropology. American Anthropologist, 120(3), 560–565.
Nakray, K. (2013). Gender-based violence and public health: international perspectives on budgets and policies. Taylor and Francis.
Phaa.net.au. (2021). Retrieved 24 March 2021, from https://www.phaa.net.au/documents/item/875
ray Jamieson, G. (2012). Reaching for health: the australian women's health movement and public policy. ANU E Press.
Vasilevska, M., Ross, S. A., Gesink, D., & Fisman, D. N. (2012). Relative risk of cervical cancer in indigenous women in australia, canada, new zealand, and the united states: a systematic review and meta-analysis. Journal of Public Health Policy, 33(2), 148–164.
Wohler, Y., & Dantas, J. A. (2017). Barriers accessing mental health services among culturally and linguistically diverse (cald) immigrant women in australia: policy implications. Journal of Immigrant and Minority Health, 19(3), 697–701.
PSYC20036 Assignment 3 Sample
Question
Reflective journal Task Description In Assessment 3, you will write a reflective journal to chronicle your reflections, insights, and ongoing development of knowledge and skills regarding the implementation of a self administered positive psychology intervention for Assessment 2. You will produce two reflective practice journal entries (600 words each, +/- 10%) documenting: • your growing understanding of how to design, implement, and evaluate positive psychology interventions in an applied setting. This will include personal reflection on why the specific positive psychology intervention was expected to be useful to your own personal or work circumstances. • evaluation of changes in perceptions, beliefs, and behaviour during the self administered positive psychology intervention. What have you noticed about yourself, your emotions, relationships, or other aspects of your wellbeing since undertaking the intervention? • reflections on progress and challenges in implementing and completing a self administered positive psychology intervention. What specific challenges did you face or how did you ensure that you continued to implement the specific aspects of the intervention? It is expected that you will relate your experiences (e.g., challenges, progress, outcomes) to what the positive psychology literature tells us about the particular intervention and, more generally, processes of change. While you will submit both journal entries at the same time, it is recommended that the first be written within the first 2 weeks of beginning your intervention and the second be written at the end of the intervention/shortly after completion of the intervention. Maximum word count: 600 words (+/- 10%) per entry. This word limit includes in-text citations but excludes any reference section. Meeting the assignment help word count is included as a part of the marking criteria in your marking rubric on Moodle. See the Psychology Word Count Information document on Moodle for a rationale for using this type of word limit restriction.
Solution
Journal entry One
The positive psychological intervention has always been one of the most powerful aspects for the development of individuals and it has focused on the overall development through building the consciousness and sense of power among all the individuals in a definite manner. I would like to discuss different aspects that are very important for my overall development in both the personal and professional aspects. The implementation of the psychological behavioral strategies for the betterment (Donaldson, Lee & Donaldson, 2019). The self-administered strategies will need to be implemented for the best results in this scenario. The treatment types of structured counseling would be very relevant to the challenges that could be addressed. Throughout this positive psychology intervention, I have found that I am not much extrovert and I like to keep shy (White, Uttl & Holder, 2019).
I understood that this habit should have to be changed so the best outcomes could be addressed. This would also help me to understand how I would communicate better with everyone in the society and workplace. To achieve better results, I should have indulged in different meditation methods and feel gratitude for everyone who has helped me in this entire process. I also came to know that I have to give my efforts to different acts of kindness (Pawelski, 2020). I have to maintain a proper relationship with everyone in society so I can ask for assistance whenever I need them. I have to present my best possible self mine so I can become what I have always wanted. I have to undertake assessments of my strengths and weaknesses. I should build the leadership components within me because this will help me to achieve the best results in the future (White, Uttl & Holder, 2019).
Psychology has come up as one of the most impactful aspects for the growth and development of individuals. This is the reason why I should learn to be optimistic all the time. This would guide me to be strong everytime (Donaldson, Lee & Donaldson, 2019).The impact of positive emotions is always high on human minds and I have felt it all the time. I believe that I should perform the best roles as a human being when I can see everything positive in the other human beings. I should learn to appreciate the efforts put in by others for the betterment of all the fields. If I appreciate them, I will get them back when I try to put in some effort. I focused on my well-being and how I can achieve it despite so many challenges (Carr et al., 2020). I was not able to lead my team effectively and get the highest sales figures. This is when I began to understand how I should try to be optimistic and influence all the team members to work collaboratively and spread the light of positivity through their works. These positive vibes have always helped me to understand different factors about success.
I will need to think of these aspects and cater to the needs of the time. I feel that the gratitude visit intervention is very important for me because this always helps in the improvement of communication in different ways. I indulged in the self-guided happiness exercises after watching videos on YouTube. It helped me to gain lots of positive vibes and I want to improve my skills and capacities to become a better person altogether. I believe this will surely help me to understand the points of understanding the relevance of showing gratitude to everyone (Woodworth et al., 2017).I felt very good and my mind was full of joy when I was doing all of these exercises. I would also continue this exercise to be my positive self.
Journal Entry Two
In this journal entry, I would describe the positive psychology intervention and how I have faced the challenges only to overcome them fruitfully. In the meantime, I had very little confidence about the works that I was going to undertake. This is why I wanted to provide more efforts to become successful in all the cases. I had to rely on my understanding and knowledge I have. I was not able to understand how I could boost up my confidence for the best outcomes (Carr et al., 2020). I have had the aim of performing at my very best so I could follow the proper process and get the best outcomes wherever needed. The above journal entry was at the beginning and during the time of positive psychology intervention. In this second journal entry, I would like to describe the aftermath of completing these positive psychology interventions. I would like to say after two months of completion of this intervention that I have been greatly benefitted from all of these strategies (Woodworth et al., 2021).
It has helped me a lot to understand how important it is to deliver the best performance by being confident and implementing the best strategies for the improvement of individual capacities. Through developing the best possible self, I have become all the more confident about my ideas. I am also able to align between my ideas and the potential strategies that I would like to execute (Proctor, 2017). I have gained knowledge about the importance of teamwork in different aspects indeed. I have become more helpful in all the works that I have participated in. Previously, I became morose after every failure and did not dare to get back stronger. Now, after this positive psychology intervention, I have highlighted the idea that I would be able to get more support from everybody around me if I show the same support to others (Gander, Proyer & Ruch, 2016). This would make the entire collaboration happier all the time. I have become more energetic about my projects and I can complete them with full authority.
These aspects have changed my life forever through positive psychology interventions. The practice of gratitude also helped me to understand that I can become one of the most successful persons in the world if I can deliver all of my works in my personal and professional lives with full confidence (Donaldson, Lee & Donaldson, 2019). I have improved my confidence and capabilities through daily strength awareness measures as well. I have gained several traits that would later help me out to become a better human individual. Some of these traits are humanity, courage, and wisdom. These traits have helped me to treat people differently and understand their challenges in life. I have become more sympathetic than before and I like to help people out in their difficult times (Gander, Proyer & Ruch, 2016)
I believe this will lead me to become a successful leader in my professional workplace. Otherwise, I cannot shine and survive in my professional career if I do not possess all of these traits. These are some strengths that I have found within myself. I am relentlessly trying to provide my best efforts and improve my performance (Donaldson, Lee & Donaldson, 2019).I have made self-administered tests and identified all the potential challenges that I still have. I will look forward to improving on my capacities that could give me a better place in society also (Woodworth et al., 2021).I felt that the stress level has reduced and I can take the decisions very calmly as well. I am more flexible in my cognitive responses. All of these factors have guided me to improve my position and status within society.
References
Carr, A., Cullen, K., Keeney, C., Canning, C., Mooney, O., Chinseallaigh, E., & O’Dowd, A. (2020). Effectiveness of positive psychology interventions: a systematic review and meta-analysis. The Journal of Positive Psychology, 1-21.
Donaldson, S. I., Lee, J. Y., & Donaldson, S. I. (2019). Evaluating positive psychology interventions at work: A systematic review and meta-analysis. International Journal of Applied Positive Psychology, 4(3), 113-134.
Donaldson, S. I., Lee, J. Y., & Donaldson, S. I. (2019). The effectiveness of positive psychology interventions in the workplace: A theory-driven evaluation approach. Theoretical approaches to multi-cultural positive psychological interventions, 115-159.
Gander, F., Proyer, R. T., & Ruch, W. (2016). Positive psychology interventions addressing pleasure, engagement, meaning, positive relationships, and accomplishment increase well-being and ameliorate depressive symptoms: A randomized, placebo-controlled online study. Frontiers in psychology, 7, 686.
Moskowitz, J. T., Cheung, E. O., Freedman, M., Fernando, C., Zhang, M. W., Huffman, J. C., & Addington, E. L. (2021). Measuring positive emotion outcomes in positive psychology interventions: a literature review. Emotion Review, 13(1), 60-73.
Pawelski, J. O. (2020). The elements model: toward a new generation of positive psychology interventions. The Journal of Positive Psychology, 15(5), 675-679.
Proctor, C. (Ed.). (2017). Positive psychology interventions in practice. Springer.
White, C. A., Uttl, B., & Holder, M. D. (2019). Meta-analyses of positive ps ychology interventions: The effects are much smaller than previously reported. PloS one, 14(5), e0216588.
Woodworth, R. J., O'Brien?Malone, A., Diamond, M. R., & Schüz, B. (2017). Web?Based Positive Psychology Interventions: A Reexamination of Effectiveness. Journal of Clinical Psychology, 73(3), 218-232.
NUR7003 Leadership Changing Healthcare Landscape Assignment Sample
Question
Write a 1000-word reflective assignment help of your approach to leadership,
acknowledging strengths and limitations.
You should acknowledge recent learning and how this may now be
influencing a change in your leadership behaviour
Please refer to the academic guidelines in assessment. You should:
• Attach your work to a completed front cover sheet
• Include an accurate reference list
Leadership skills enhance the communication by delivering the mission and vision of the firm to its employees very effectively. This further helps in identifying the roles which can best fit for the academic skills. Leadership techniques have helped me in understanding the influence of others and the capacity towards determining a particular goal. When the leadership techniques come into play, it can be beneficial both at the workplace for the delegation of work as well as it enhances a personal wellbeing of an individual. In my personal experience, the leadership techniques have helped me to establish effective communication and encourage the team members for the task performance. During my college days, I have observed that when working in teams, the leadership and managerial practices helped in minimising the errors and also gaining constant progress in the work. I tried to help the team members initially by setting up effective communication. In the starting of the project, I mentioned the team members that they can feel free to express their views on how to precede with the work. This gave them the confidence to further understand the work details and set up meetings which can help in the better understanding of the work.
Solution
Leadership has also helped me to improve my communication skills and to enhance my self-confidence. This can be mentioned as the way in which enthusiasm it involved. Often,I used to find it difficult to understand a certain task and would find lack of time in performing it. After I had implemented the leadership techniques, it has helped me to understand the details of the work in a far better manner. I have also been able to focus on the group activities more. Confidence is increased when the targets of the group assignments are met and the team members are satisfied with the leadership technique that had been followed for the completion of the work (John and Bertram, 1959).The main challenge that I observed during the practice of the leadership skills is that it was sort of difficult for me to comprehend my own values and principles. I would always jump to assumptions and conclusions really quick which made me fail a couple of time. Those failures were the times I learned the most. I have also observed that when the most appropriate leadership technique is not followed then the organisational complexities are increased. Similarly, Michael Hartsfield(2010) also stated, “Managers do things right and leaders do the right thing.”
Gibbs Reflective Cycle helps in encouraging people to think and reflect on the experiences they had faced during a certain situation, activity or even event. With the help of a circle, a reflection on those experiences which they went through can be structured in several phases. This I can relate to an incident when I did an internship with an organisation, there the leadership practices were not followed and it became hard for the members to understand as to how they should behave within theworkplace and how to proceed effectively with the tasks. This is the main reason why I failed in submitting most of the projects on time because that had to be done in the group activities and it was hard for the members within the team to understand as to how to discuss and delegate the different responsibilities within the project. This has helped me to become more flexible in understanding the group approaches and further lead myself into the team and help all the members to achieve progress. This incident helped me in reflecting upon the skills that I never thought I inherited. The next course of action would be to enroll in courses related to leadership that could enhance my managerial skills and abilities in order to effectively manage change and nurture the people around me.
.png)
Figure 1: Gibbs reflective cycle
(Source: Mindtools, 2022)
The four E’s framework also been a great help to me for identifying the actual context of leadership in the global concern and to differentiate within the national and the global leadership techniques. These includes the energy, energising ways, the edge of the technique which is considered for moving ahead with the leadership practice, the way of execution of the leadership technique which can be beneficial for an individual or the organisation. Passion of the leader is also considered in the global context where the work proceedings of the leader are considered. Here the passion of the leader is noted as to how they try to manage the team and follow the guidelines of the workplace and how far they are successful in making the team understand about the work details (David, 2012). The way they try to manage the working of the team, support them in time of need and further guide them with the necessary training and support as required can help the leaders to maintain the leadership technique which is appreciated by the people.
.png)
Figure 2: 4 E’s framework
(Source: Researchgate, 2022)
There are several approaches to leadership as well which also contains the ethical norms. As stated by French & Raven, the power bass procedures are handled when it comes to understanding the stakeholders care and the ethical concerns (Alan & James, 2018).As stated by Yukl and Yukl,ethical leadership technique also played a great role in building my leadership skills. The ethical values consider the practices such as trustworthiness, honesty and responsibility. When I tried reading the leadership approaches, it helped me to understand the benefits of being more honest and trustworthy within the workplace or in any group activity. When such practices are considered, it has not only helped me to increase the transparency in the group activities but has further helped me to understand the ways in which the team can be managed. When I asked the team members to be honest regarding their work, they tried to provide me the details and the areas which they find it hard to understand.
Therefore, it can be stated that following of the leadership techniques can not only help in better performance at workplace but can further help in making the team more authentic. My self-confidence has been boosted after the utilisation of the leadership practices as I got much appreciationregarding the team work. I also got the support of my team members in the work proceedings and they also tried to help me in times of need which further made our team strong. Hence, I would like to conclude that the best leadership technique suitable for the workplace needs to be considered for the development of an individual as well as the team.
References
Michael, H (2010). Leadership Reflection: Leaders Do the Right Thing: A Popular Phrase or a Real Practice?https://www.regent.edu/journal/journal-of-biblical-perspectives-in-leadership/leaders-do-the-right-thing/
Alan, C. and James, S. (2018) Sources of Leadership Power - French and Ravenhttps://www.businessballs.com/leadership-philosophies/sources-of-leadership-power-french-and-raven/
John, R. and Bertram,R. (1959) The Bases of Social Powerhttp://www.communicationcache.com/uploads/1/0/8/8/10887248/the_bases_of_social_power_-_chapter_20_-_1959.pdf
David, C. (2012) Continuing Confusion -Are Managers and Leaders Different?https://scholars.fhsu.edu/cgi/viewcontent.cgi?article=1047&context=jbl
Researchgate, (2022) 4 E’s framework https://www.researchgate.net/figure/The-4Es-model-for-delivering-behavioural-change_fig1_284187722 (Accessed on March 23, 2022)
Mindtools, (2022) Gibbs reflective cycle.https://www.mindtools.com/pages/article/reflective-cycle.htm (Accessed on March 23, 2022)
GDECE101 Early Childhood Care and Education
Assessment 1:
Essay (1000 words) Inclusive strategies and approaches when working with careers/families and communities. Inclusive strategies and approaches when working with carers/families and communities.
Following the guidelines in the EYLF and the NQF, review a range of contemporary inclusive approaches and strategies related to working inclusively with carers/families and communities.
Compare and contrast the recommended practices with some of the historical approaches examined in class.
Please use the APA referencing style.
Weighting - 50%
Learning outcomes
On successful completion of this subject you will be able to:
A. Evaluate historical constructs of childhood and their impact on contemporary early childhood systems and curriculum in Australia.
B. Assess a range of strategies for promoting effective and respectful working relationships with diverse parents/carers and communities.
C. Debate contemporary educational issues in social, cultural, political, philosophical and historical contexts.
D. Appraise diverse Indigenous Australian and Torres Strait issues and epistemologies and their impact on early childhood care and education.
E. Advocate for children’s rights and anti-bias approaches to working with diverse cultures and identities.
Solution
EARLY CHILDHOOD CARE AND EDUCATION
Introduction
Early learning frameworks for the student help in maintaining a holistic approach to the parents for understanding the needs of their child. In this assignment there are detailed strategies for promoting the impact of learning.
Contemporary childhood systems and curriculum
National Quality Framework and Early Years Learning Framework help to create better childcare systems and regulations to maintain an understanding among the caregivers or the families to convey the need of improvement in a child. These two contemporary systems work for a long time to sustain a developmental aspect on the child’s health and mental development (Hamilton et al. 2019). In historical context early stage of student’s development is divided into series of stages such as preoperational or sensory motor operation development. In early education system a common goal of student development is to sustain a better development of the mental health of students at an early age (Petit Early Learning Journey, 2019). Academic success and continuation to traditional process may differ in different countries. Nowadays childcare curriculum is divided into theme based, high scope based and Montessori based.
Theoretical Overview of NQF and EYLF
NQF:
The National Quality Framework, or NQF, established by the Australian Government, regulates the education provision for early childhood and promotes children's first five years’ education (Ghoghra, 2017). NQF includes:
National Quality Standards
National legislation and national legislation.
National Education Framework.
Evaluation and Quality Assurance Process
.png)
NQF
Source: (Petit Early Learning Journey, 2019)
The first impetus for change began with the COAG or Australian Government Council meeting in December 2007. They agreed to make "significant improvements in the educational areas, skills and development at early childhood ". The 2008 discussion paper 'National Framework for Early Childhood Education and Care' explains the reasons for these changes. These revealed that:
? More working parents are starting to work in Australia
? Increased compulsion to provide for families
? Providing high-quality care to multiple children:
? Significant benefits for disadvantaged children
? Improving short-term outcomes such as school readiness
? Less risk of abduction of "vulnerable" children.
? More classroom diversity.
? Establishing a healthy lifestyle and learning
? Significant social and economic benefits
? Differences and gaps in the rules for quality identification, assessment and monitoring in care and education across Australia.
? Removing inappropriate differences between education and care sectors create divisions between child care and kindergarten sectors.
? The children should be the priority above all (Petit Early Learning Journey, 2019).
EYLF:
The EYLF is the first Australian framework of national curriculum for education at early childhood. It emphasizes activities that are play-based to improve early childhood education and the significance of language communication (including early numeracy and literacy). In July 2009, the COAG approved five learning outcomes for children ages 0 to 5 as part of the EYLF and structured according to the following related factors: theory, practice, learning outcomes (Ghoghra, 2017).
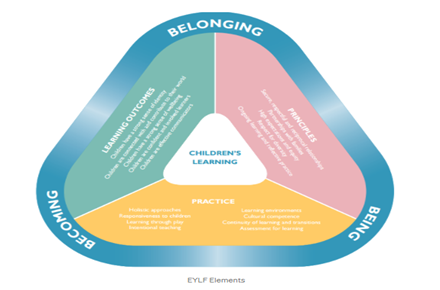
EYLF Framework:
Source: (Ghoghra, 2017)
The framework is based on a vision of children's health characterized by participation, attendance and presence. Children at early stage are mostly connected to community, family, environment and culture. (Ghoghra, 2017).
Belonging: The experience of being a part and is an important part of one's life. Children are part of a cultural group, a family, and an entire community. Being: Childhood is a time to understand, explore and understand the world. Being a child recognizes the value of life in the here and now. Childhood is a preparation not only for the future but also for the present (Ghoghra, 2017).
Becoming: Children's knowledge, relationships identities, abilities &skills, and understanding change during childhood. Strategies of effective relationship
Discovering Identity: Strong sense of identity is another important part for parents in the early age of their children’s of the development. It helps working parents to get a good grasp on identifying the strengths and weaknesses of their children. The EYLF system helps to maintain a proper understanding of the importance of the development of the child system (Quality forum, 2021). Identity development is an essential phenomenon for the growing children for further development.
Connection and Contribution: In order to feel the connection to their external and internal environment it is essential for parents to keep their children in a good situation. It helps to create a better understanding to the children and they can easily learn where to contribute their intelligence. They can generate a strong sense of their rights and community values as well (Press et al. 2018).
The aims of education have different problems in clarification and it is needed to be mitigated quickly.
Mitigating problems and issues of Child care
Strategic plans have been developed for maintaining a better understanding of the indifferent development of the children in a positive environment. NQF and EYLF both have their own version of distinctive plans for nurturing children of working parents (Morrissey & Moore, 2021). Family engagement and care: It is an important step for strategic planning of the child care systems to maintain values to the care systems which in turn helps to the development of the child. They help to generate the thinking skills with the medium of play based learning systems (Hamilton et al. 2019). Mitigating quality gaps: It is important to maintain a better place without any discrimination at an early age. It is important to create awareness from an early childhood to maintain a discrimination free mentality. As “charity begins at home” it is important for parents to maintain these critical aspects of life and respect each other that can develop the mind of a child.
Leadership development: It is another important phenomenon of the child care units to develop the integrity of doing work that can help children in future. Sustainability: It is important for every family to care for their children from any harm whether it is external or internal. It is an important step for a family to maintain such understanding for better development of their children (Petit journey, 2021).
Conclusion
Strategic plans for the parents and the caregivers to create a sustainable environment for the children to thrive upon. It creates an understandable environment for the children and the family both.
Reference list
Ghoghra, R. D. (2017, June 21). NQF, NQS and EYLF. Retrieved November 25, 2021, from Medium website: https://medium.com/@riya.ghoghra/nqf-nqs-and-eylf-2e392cdfc440
Hamilton, A., Jin, Y., & Krieg, S. (2019). Early childhood arts curriculum: a cross-cultural study. Journal of Curriculum Studies, 51(5), 698-714. Retrieved on: 12th November 2021, from; https://www.researchgate.net/profile/Yan-Jin-17/publication/330949330_Early_childhood_arts_curriculum_a_cross-cultural_study/links/5ce0db2892851c4eabacede4/Early-childhood-arts-curriculum-a-cross-cultural-study.pdf
Morrissey, A. M., & Moore, D. (2021). In whose best interests? Regulating childcare environments in Australia. Australasian Journal of Early Childhood, 18369391211050184. Retrieved on: 14th November 2021, from; https://www.researchgate.net/profile/Anne-Marie-Morrissey-2/publication/355318538_In_whose_best_interests_Regulating_childcare_environments_in_Australia/links/6171623f766c4a211c04f0b1/In-whose-best-interests-Regulating-childcare-environments-in-Australia.pdf
Petit Early Learning Journey. (2019, April 29). What is the Early Years Learning Framework? Retrieved November 25, 2021, from Petit Journey website: https://www.petitjourney.com.au/early-years-learning-framework/
Press, F., Woodrow, C., Logan, H., & Mitchell, L. (2018). Can we belong in a neo-liberal world? Neo-liberalism in early childhood education and care policy in Australia and New Zealand. Contemporary Issues in Early Childhood, 19(4), 328-339. Retrieved on: 14thNovember 2021, from; https://researchoutput.csu.edu.au/files/26276662/22831996_published_article.pdf
Quality forum (2021), A Strategic Plan for Achieving the Care We Need, Retrieved on: 14th November 2021, from; https://www.qualityforum.org/A_Strategic_Plan_for_Achieving_The_Care_We_Need.aspx
HEALT1113 Effective Communication For Health Professionals Assignment Help
Due Date: Wednesday, 6th April 2022 - 23:59 hour (Week 6)
Value of the Task: 30%
Word Limit: 1800 +/- 10%
Assessment Details:
Building on your understanding of effective communication from Task 1a, you will explore effective communication with patients using a case study. You will assume the role of a Registered Nurse, a Physiotherapist or an Occupational Therapist, who has received a client referral for patient management with the focus on effective communication. You have not yet met this patient/client. You should critically reflect on how communication with the patient/client will take place. You must choose ONE of the two cases provided in Moodle for your essay response.
Assessment Structure for essay writing help
Your essay must include the following:
1. Introduction (10 -15% of total length).
a. Introduce the concept of effective communication in your specific health context
b. Provide an overview of the case study you have chosen.
c. Outline the main points you will discuss in the body paragraphs
d. Use in-text citations and ensure they are reflected in the reference list.
2. Body paragraphs (5 paragraphs)
HEALT 1113 – Effective Communication for Health Professionals - Assessment a. Using the headings and prompts as a guide provided in the essay template, create complete paragraphs applying academic writing style, plus evidence to support your claims using in-text citations.
b. Highlight important elements from the case study that will determine your communication strategies
c. Your writing should include analysis and synthesis of the research.
3. Conclusion (10% of total length)
4. Reference list: APA 7th edition
a. You are required to reference a minimum of eight academic sources (e.g. textbooks, peer reviewed journal articles).
b. Resources such as websites, legislations, and government sites are in addition to the minimum of eight academic resources.
c. Reference list is NOT included in the word count, but in-text citations are included in the word count.
Solution
Introduction:
Communication has been playing a major necessary and critical role in the field of healthcare as it ensures health care professionalssustain a position to understand patient needs, the issues as well as involve them through the process of effective care and treatment process. Patient with misuse disorder of alcohol or any other substances often sustains addictive behaviour and related medical issues or comorbidities (Ratna, 2019). Thus, it explains the need for effective treatment and care for the patient, in order to provide better and accurate treatment and recovery options to the patients, it is essential to understand the underlying factors such as the reason behind the addiction, the difficulties witnesses post addiction as well as the better options available. In such conditions, communication plays a significant role in assessing the patient as well as planning for a better treatment plan involving the patient themselves (Prip et al., 2018). The essay will focus on the case study of a 19 years old Maggie with a state of alcohol abuse and associated complication. In this essay, the different communication goals for the patient, communication strategies, along with potentialbarriers to effectivecommunication and interprofessionalcommunication related to Maggie’s case study will be evaluated using a perspective and critical role possess by a registered nurse.
Body:
Focusing on the case study of Maggie, a few significant communication goals have beendeveloped in order to ensure better treatment and recovery outcomes. One of the effectivegoals of communication in the case of Maggie is to generate awareness about the issue she has been witnessing in terms of her alcohol abuse. Health communication is known to be the study and practice of communicating with the aim to promote health information (Finset et al., 2020). It focuses on guiding and educating the community, public or patients in terms of their illnesses impacts and treatment needs with increased health literacy. Another communication goal for Maggie will focus on developing therapeutic communication in order to involve her in the treatment process and initiate a patient-centred approach to care and treatment (Martin & Chanda, 2016). The main aim of therapeutic communication is to help and assist professionals such as nurses and clinicians in developing trust and a therapeutic bond with the patient. It assists them in developing a collaborative approach with patients and another interprofessional team in order to ensure the physical and emotional involvement of the patient in their own treatment and recovery process (Schwind et al., 2016). It also serves as a way to understand the issues faced by the patient in terms of both their mental and physical health. Thus, focusing on the issue faced by Maggie, the communication goals will help in seeking a better understanding of the issue and difficulties she faces as well as developing a treatment and care plan according toher needs and demands during the treatment and recovery.
Focusing on the case study of Maggie and the communication goals addressing her issues, it will be necessary that certain communication strategies are involved in the care plan in order to ensure better communication establishment and treatment outcome. One of the necessarycommunicationstrategies in the case of Maggie accounts for active listening in orderto evaluate the issue she has been witnessing and the reason behind her difficulties. Active listening serves a crucial and essential role in the entire process of communication as it aims at addressing the significant process of receiving as well as interpreting information provided (Jahromi et al., 2016). It providesanopportunityto understand the chief research behind the progression of the issue as well as understanding patient needs. As Maggie has been identified to be becoming withdrawn and has sustained a state of loneliness along with mood issues in her life due to difficulty communicating with family as well as lacking friends, active listening is one of the necessary strategies that must be included in the communication process. Another significant communication strategy that needs to be incorporated into their treatment and care plan for Maggie accounts for patient teach back. It is one of the necessary and significant communication strategies in their field of health care where nurses and physicians focus on effectively communicating and making understanding information to the patients (Yen &Leasure, 2019). Often patient says they have understood everything guided by the nurses or the physician but the majority of the information is either neglected or not understood by the patient. Thus, in such conditions patients are enquired to repeat along with the professional and often requested to state what they have understood as a way of taking back in terms of communication (Talevski et al., 2020). Thus, it will be used as a process of communication strategy where after ensuring communicationandinformationdeliveryMaggie will be guided through the process of taking back communication. In order to implement these effectivecommunicationstrategies in the care and treatment process of Maggie, a patient-centred approach to communication must be incorporated. In the approach, the nurse or physician focuses on providing care and treatment based on patient values, beliefs, needs as well as preferences such as her need to have better diet, to indulge in physical activity and to communicate with community members to overcome the issue Maggie is currently facing. Focusing on her need, it is necessary to communicate with someone, as it helps her to overcome the sleep disorder, mood disorder and will also help to gain effective weight (Schembre et al., 2018).It aims in involving the patient in active participation in the whole process of communication, treatment plan and recovery services (Wolters et al., 2017).
In order to address Maggie and ensure her involvement of her in the treatment and care process focused on effective communication, it is necessary that a positive rapport is built with her. Building rapport will ensure sustaining her trust and active participation in the process of treatment as she is known to witness withdrawal from family and friends and is in a state of loneliness. (Barkley, 2016) She also was found to lack interest in talking to anyone and remain in her own space with changing mood issues It is one of the chief reasons behind her state of addiction as she drinks more to remove her loneliness and sustain sound sleep. Focusing on the needs, the BATHE protocol of effective communication will be used in order to build rapport with Maggie. It is one of the significant and useful strategiesin the case of health care where professionals are provided with an opportunity to build rapport with their patients and extract them out of suffering to ensure ease and comfort (Pace et al., 2017). It focuses on open-endedinteractionand communication with the patient with an aim to build effective and strong relationships which do not always limitto clinical needs. It helps in understanding the patient’s identity, individuality, traumatic situation, distress experiences, difficulties, issues as well as diverse health needs. It does not focus on reliving the health issue but aims to ensure activelisteningand developing a significant therapeutic and interactive bond with the patient (Chengappa et al., 2020).
The BATHE protocol focuses on 5 stages which include
? Background – about patients and their life
? Affect – the impact of the findings on the patient
? Troubles – issues that the patient is witnessing
? Handling – the way the patient is handling the situation
? Empathetic Statement – show empathy and respect to the patient ensuing different consoling sentences.
Potential communication barriers
After going through the case study and the factors involved in the issues witnessed by Maggie, it has been foundthatthere are two potential barriers that may develop in their process of effective communication. One of the factors accounts for emotional barriers where patient emotional values and conditions often develop a hurdle in establishingeffectivecommunication. Emotions such as anger and lonelinessoftendevelop a wall between the patient and the communication as the patient’s emotional distress keeps them deprived of the ability to understand and evaluate the aim of communication (Mack et al., 2021). As Maggie has been witnessingmooddistress, due to lonelinessas well as a lack of ability to interact with her parents. A state of emotional barrier in communication may develop as she does not sustain the interest or intention to communicate with others. Also, it has dragged her towards the state of increasedalcoholconsumption as it helps her to get through the day and have a sound sleep at night. Thus, in such conditions, it is necessary that effective therapeutic communication must be focused on where initially a rapport is built with the patient in terms of trust and respect (Blake & Blake, 2019). It will help the patent to open up to the professionals and deal with the emotional barrier to communication. Also, in the case of involving her mother in the treatment and care plan focusing on a patient-centred approach, a potential social-cultural barrier to communication might develop (Schouten et al., 2020). Due to having cultural differences and a bad experience in health care due to belonging to the Aboriginal community, her mother hasa state of untrustful interest in healthcare facilities. Maggie belongs to the Aboriginal community and the care process involved themother as next to the kin, thus focusing on their cultural values, culturally safe and sensitive communication must be involved. Thus, it also might develop a potential barrier in the communication process and to resolve and overcome the barrier, it will be necessary to focus on involving culturally safe communication (Brooks, Manias & Bloomer, 2019). Focusing on the cultural diversity of health care settings, often communication must focus on a culturally sensitive and safe process. It will focus on ensuring a communication where the divert of the patient's culture, values and perspectives will be respected and maintained in their communication and treatment process.
In the case of Maggie's treatment plan, professionals such as Psychologists for mood disorders such as changing mod patterns as well as alcohol abuse, the dietitian for loss of weight and inability to eat as well as a family counsellor for the disruptedinteractionand communicationbetweenMaggie and her mother. These three professionals apart fromregistered nurse will be involved and communicated in the treatment plan for Maggie. In case of effective communication with healthcare professionals belonging to different healthcare backgrounds and specializations, it is necessary to ensure clear and accurate communication. It will be necessary to focus on written communication along with interprofessional communication to ensure proper sharing of evidence without the conduction of error (Wei et al., 2022). Often challenges such as diversity in professional dynamic may develop as each professional belongs to a different professional background along with a lack of understanding of their role in their interprofessional collaboration. Thus, in such conditions, an effective collaborative approach with significant interprofessional communication is necessary to overcome these challenges (Chichirez&Purc?rea, 2018). It will help in understanding the dynamics of each professional as well as ensuring sharing of information and understanding related to their role in the treatment plan.
Conclusion:
The essay was to assess the differentcommunicationstrategies and their impact on the case study of Maggie as she has been identified to be suffering from mood and alcoholmisuseissues. After completion of the essay, it has been found that Maggie has explained the need for effective communication in her treatment andrecovery plan as one of the major issues that she faced was a lack of interaction with her family. It dragged her towardsalcoholmisuse, and thus focusing in which, the essay highlights the significant communication gaols and strategies that must be provided to her in order to restore her cognitive and physical health back to normal. The essay helped in assessing the different type of communication strategies as well as their need in healthcare. It also helped in evaluating the type of professionals and professional communication that must be maintained while assisting a patient with alcohol misuse disorder.
References:
Barkley, P. S. (2016). Building rapport with your patient: Positive case management outcomes. http://ocu.course.documentation.s3.amazonaws.com/HS2800/WK1+Building+Rapport+with+your+Patient.pdf
Blake, T., & Blake, T. (2019). Improving therapeutic communication in nursing through simulation exercise. Teaching and Learning in Nursing, 14(4), 260-264. https://doi.org/10.1016/j.teln.2019.06.003
Brooks, L. A., Manias, E., & Bloomer, M. J. (2019). Culturally sensitive communication in healthcare: A concept analysis. Collegian, 26(3), 383-391. https://doi.org/10.1016/j.colegn.2018.09.007
Chengappa, N., Honest, P. C. R., David, K., Pricilla, R. A., Rahman, S. M., & Rebecca, G. (2020). Effect of BATHE interview technique on patient satisfaction in an ambulatory family medicine centre in South India. Family Medicine and Community Health, 8(4). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7566425/
Chichirez, C. M., &Purc?rea, V. L. (2018). Interpersonal communication in healthcare. Journal of medicine and life, 11(2), 119. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6101690/pdf/JMedLife-11-119.pdf
Finset, A., Bosworth, H., Butow, P., Gulbrandsen, P., Hulsman, R. L., Pieterse, A. H., ... & van Weert, J. (2020). Effective health communication–a key factor in fighting the COVID-19 pandemic. Patient education and counseling, 103(5), 873. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7180027/
Jahromi, V. K., Tabatabaee, S. S., Abdar, Z. E., &Rajabi, M. (2016). Active listening: The key of successful communication in hospital managers. Electronic physician, 8(3), 2123. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4844478/
Mack, J. W., Currie, E. R., Martello, V., Gittzus, J., Isack, A., Fisher, L., ... &Bakitas, M. (2021). Barriers to optimal end-of-life care for adolescents and young adults with cancer: bereaved caregiver perspectives. Journal of the National Comprehensive Cancer Network, 19(5), 528-533. https://doi.org/10.6004/jnccn.2020.7645
Martin, C. T., & Chanda, N. (2016). Mental health clinical simulation: therapeutic communication. Clinical Simulation in Nursing, 12(6), 209-214. https://doi.org/10.1016/j.ecns.2016.02.007
Pace, E. J., Somerville, N. J., Enyioha, C., Allen, J. P., Lemon, L. C., & Allen, C. W. (2017). Effects of a brief psychosocial intervention on inpatient satisfaction: An RCT. Family medicine, 49(9), 675. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5689450/
Prip, A., Møller, K. A., Nielsen, D. L., Jarden, M., Olsen, M. H., & Danielsen, A. K. (2018). The patient–healthcare professional relationship and communication in the oncology outpatient setting: a systematic review. Cancer nursing, 41(5), E11. https://doi10.1097/NCC.0000000000000533
Ratna, H. (2019). The importance of effective communication in healthcare practice. Harvard Public Health Review, 23, 1-6.https://www.jstor.org/stable/48546767
Schembre, S.M., Liao, Y., Robertson, M.C., Dunton, G.F., Kerr, J., Haffey, M.E., Burnett, T., Basen-Engquist, K. and Hicklen, R.S., 2018. Just-in-time feedback in diet and physical activity interventions: systematic review and practical design framework. Journal of medical Internet research, 20(3), p.e8701.https://www.jmir.org/2018/3/e106/
Schouten, B. C., Cox, A., Duran, G., Kerremans, K., Banning, L. K., Lahdidioui, A., ... &Krystallidou, D. (2020). Mitigating language and cultural barriers in healthcare communication: Toward a holistic approach. Patient Education and Counseling, 103(12), 2604-2608. https://doi.org/10.1016/j.pec.2020.05.001
Schwind, J. K., McCay, E., Metersky, K., & Martin, J. (2016). Development and implementation of an advanced therapeutic communication course: An interprofessional collaboration. Journal of Nursing Education, 55(10), 592-597. https://doi.org/10.3928/01484834-20160914-11
Talevski, J., Wong Shee, A., Rasmussen, B., Kemp, G., & Beauchamp, A. (2020). Teach-back: A systematic review of implementation and impacts. PLoS One, 15(4), e0231350. https://doi.org/10.1371/journal.pone.0231350
Wei, H., Horns, P., Sears, S. F., Huang, K., Smith, C. M., & Wei, T. L. (2022). A systematic meta-review of systematic reviews about interprofessional collaboration: facilitators, barriers, and outcomes. Journal of Interprofessional Care, 1-15. https://doi.org/10.1080/13561820.2021.1973975
Wolters, M., van Hulten, R., Blom, L., &Bouvy, M. L. (2017). Exploring the concept of patient centred communication for the pharmacy practice. International journal of clinical pharmacy, 39(6), 1145-1156. https://doi.org/10.1007/s11096-017-0508-5
Yen, P. H., &Leasure, A. R. (2019). Use and effectiveness of the teach-back method in patient education and health outcomes. Federal practitioner, 36(6), 284. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6590951/
PBHL20004 Public Health Action and Evaluation Assignment Sample
This is an INDIVIDUAL assessment. Based on your informal reflections throughout the term, you will explore your ability to develop effective partnerships with others, including establishing relationships and collaborative learning. In a 1500-word essay, reflect on your group partnership throughout the term. In your essay, you will need to focus on following points for assignment help:
• The group process in establishing and maintaining relationships throughout the term
• The effectiveness and experience of collaborative learning within the group
• The relevance of this experience in undertaking community-based public health actions and evaluations.
A minimum of two appropriately cited references is required.
Solution
Introduction
The reflective assessment will shed light on the team dynamic and how my personal growth is determined by collaborative learning within the team. It will also be demonstrated how the relevant experience will be conducive to the effectiveness of healthcare practices that are based on values and ethics.
Discussion
The group process is one of the relevant activities to maintaining relationships. I think maintaining bonds with members of the team is key to professional efficiency. Productivity is guaranteed only when there is no miscommunication in the team. Group partnerships uplift confidence, and make morale strong. I always look forward to fruitful learning that becomes easier to communicate with the team members in a friendly spirit. The group process instils the spirit of togetherness that sharpens the intellect and cognitive powers to flourish to the fullest (Van Leeuwen and Janssen, 2019). Unity in the entire team is very much required that keeps the team going toward the desired destination. At the same time, it channels the energy in a positive direction. I have learned how to stay connected with other people at a critical juncture. Personal connectivity enriches the professional outlook that makes the output attuned to the purpose. The more connections that can be developed within a team, the more growth one can achieve through the discussion. Many people being assembled in one place contribute to the knowledge by sharing valuable opinions on a particular topic. The various perspectives generate strong individual insights and paradigms (Qureshi et al., 2021). The exchange of cultural values and the discussions pave the way for the comprehension of the multiple topics and the various usages of these into the perfect application.
I have enhanced my decision-making process having been involved with team collaboration and dynamics. My leadership qualities have been made to tackle a situation with dexterity. Professional growth has been fuelled by personal determiners. I have comprehended one process that socialisation is being made easier by maintaining relationships with the team in a friendly manner. A positive outlook has grown that removes all complications and odds. Simple manners and outlooks have grown to be developed while discussing with peers. I have highly benefited from the multiple views of different people or cross-cultural ethos, differences and symptoms. The team undertaking the task to finish, it is not difficult to finish the task with alacrity and promptness (Ansari and Khan, 2020). Group thinking has enhanced my analytical skills and this is necessary for the increase of patience, determination, and composure. Without chaos, the decision-making process gets more stable and appropriate to the condition. Contextualisation makes learning fast and effective. Different needs of the individual get fulfilled and when the opinion is asserted, it keeps all the inhibitions at bay. All the insecurities can be dissolved and this is the cornerstone of overcoming challenges with a smile (Van Leeuwen and Janssen, 2019). I have incorporated a lot from the group process and maintained a good connection with the others. I have developed the strongest attitude having been involved in the intensive discussion. I have been insured to take more dangerous risks in my stride and that is effective for the process to be risk-free and devoid of uncertainties and indifferences. I become innovative in solving critical problems with calmness and creativity. Learning from past experiences, I have been able to head-on with the present collisions with steadfastness.
The effectiveness and experience of collaborative learning within group can improve self knowledge’s. The efficiency of collaborative learning helps me focus on my strengths and lets me categorise my weaknesses. After the weakness has been identified, I have been enabled to set up the thinking of the highest capability with strong intuition. My organisational skills have been sharpened which leads to better and proactive management of self and dexterous control over the difficulties in life. Communicational goals have been set and I have strived to the setting of the goal with purpose. The interaction will be developed to widen the scope of understanding and the knowledge objectives. I have increased my self-esteem and encouraged the other members to follow the creative pattern of thinking to shine in life. The development of interpersonal and social skills maximise the educational missions that would demonstrate the goals to the team (Florence, 2020). The chance of miscommunications, risks, and hazards will be less which promotes combative decision and continuous learning. I have been inspired to follow social interaction and dimensions that project the groups in the development of interactional skills. The creation of a diverse atmosphere helps the professionals delve into the depth of concepts and skills. The critical concepts and ideas are related to the emergence of analytical powers. I am now good at offering valid judgments. The power of constructive criticism has been developed by the capacity to influence people with courage, confidence and a people-solving mentality.
Members of the team will work for the same goals and develop the power of empathy and respect for others' feelings. Active listening makes the social skills strongest which helps the future orientation solid and fundamental. I have learned to respond to the various applications and opinions and angles. Open-mindedness has been developed that makes the connections between personal and professional skills. Through collaborative learning, I have gained the trust and learned to place credibility on the onions made by the team. The supportive ambiance will raise the optimism and the growth that are accountable for the future productivity in the group (Ansari and Khan, 2020). The learning experience has been fruitful in making the content fun-filled and true to the experience. I have felt comfortable discussing with the team members and this is effective in the origination of the inspiring content and the evaluation of the ideas in the future. The ideas of different people influence my thinking in making positive contributions.
The experience of learning collaboratively has majorly helped me in undertaking community-based public health actions. The experiences gathered by collaborative learning have helped me to understand what I can do to undertake public health actions better. The experience has given me the ability to judge the strengths and weaknesses of other members in the group. The experience can be used to assign particular sectors to a particular person who is good at it (Omae, 2021). Through using the experience of collaborative learning I and other members can learn faster about what can be done to undertake a community-based public health action. The experience also helped me to communicate my thoughts to the other members of the group which made it even easier for everyone to work towards a single goal. Utilising the experience I learned qualities of leadership which also helped me to lead a group of members in undertaking a community-based public health action. Having the experience of collaborative learning also helps everyone to be more solution-oriented rather than focusing on the problem (Florence, 2020). Through learning new things from each other I managed to be more capable to undertake community-based public health actions, the experience also helped me understand other members better.
Collaborative learning has germinated a sense of values, morality and ethics and I think this will be helpful when I will extend the hand of support to the community people. The relevance of the moments and the experience will let me know each other. It is very important to consider and treat human beings with blue and compassion. Health care demands value-given care where the patients no longer feel stressed and depressed. Community-based actions stimulate hearty efforts and these will regulate the higher concentration and morale in the work people are going to undertake. The more I will utilise the accumulated learning in the professional field, the stronger I will be. Value-based care requires the efficacy of the individual to be a good caregiver (Qureshi et al., 2021). I will be empathetic to assess the real needs of the people and offer the right kind of attention they are craving. Many patients feel estranged from the mainstream of life and they cannot reconcile with their previous experiences. The constant desire to be a part of society makes them more vulnerable and the caregivers must be affectionate enough to make them forget the loss of family and friends.
I will be at my best to question the value of being given care and learn from the entire journey. I will try to create the situation so that they again gain a renewed sense of hope and certainty in life. I will exercise the practices of ethics and morality in each complicated scenario. I will be able to manage the needs of the afflicted people and give them the promises of hope and resilience. The patients will benefit from value-based learning. The sociocultural ambiance will be justified and this will make my purpose strong.
Conclusion
This is identified from the above discussion that group-based learning adds to the dynamic benefits and positive outlooks for the participants in the tear. The reflective account has demonstrated how the gathered learning will come to help in the future period.
Reference List
HEAPH6007 Public Health Ethics Assignment Sample
Task: Health Promotion Program Plan: In this assignment – as an actual/potential health promotion professional/practitioner - you are going to explore/develop a population health promotion strategy to address an identified health need in your community that reflects the health need and target group that you identified in both Assessments 1 & 2. There are two different scenarios here. These being:
1. It may be an existing/recent comprehensive health promotion programme that you are detailing and critiquing.
2. It may be a purely 'hypothetical' (mock) example of a comprehensive health promotion that you would like to see in practice in your community.
Whichever scenario you choose - it is probably best to highlight (early on) in your assignment which option you are adopting and identifying your role within it.
Plan a program that is based on the principles of comprehensive health promotion process; including community development, community stakeholders and their various roles - and include your own role.
Your Program Plan will include:
• the background to the problem (what do we know about the problem and how to address it)
• the program goal (what you hope to achieve)
• objectives (what factors you need to address to achieve the goal)
• delivery strategies (what you are going to do)
• an evaluation plan (how you are going to know that you have been successful)
Word count - 2000 Words
Solution
Introduction
Research conveys that asthma is an international health issue though it is not much acknowledged internationally. Globally 300 million people are suffering from asthma. Extra mucus in the airways causes coughing, shortness of breath, and wheezing (Kuruvilla et al. 2019). There can be life-threatening asthma attacks for which consultation with the doctor for the person and symptoms is required. The paper thereby will share its concern for health promotion programs for asthma where it will offer a background of the problem to identify goals and objectives so that delivery strategies can be identified accordingly. An evaluation plan even will be justified to understand the success or failure of the health promotion program.
The Background of The Problem
In an emergency, a person with an asthma attack can apply some of the techniques like sitting up straight, avoiding triggers, calling the emergency number, and exercising the Buteyko breathing technique (Abrams, 2020). Due to several factors like weather changes, stress, the side effect of medication, allergies, colds, and flu, asthma can take place. Considering the illiteracy or ignorance regarding asthma and its prevalence internationally, a health promotion program for the same is much required. Understanding the causes and symptoms of asthma and its prevalence in society, it is very important to address the issue properly. As it is stated that prevention is better than cureness thereby avoiding severe asthma attacks, it is better to address the disease from its route. The health promotion program needs to focus on every possible prevention strategy to make society free from this disease as much as possible (Hartley et al. 2020). The main focus of the program needs to be acknowledgment or awareness in society regarding its severity, causes, and symptoms to be well aware of.
Program Goal
The program aims to assist people with asthma in initiating asthma control to reduce asthma rates and deaths. It even objectifies inclusive health promotion programs where communities like military members, children, pregnant women, senior adults, Hispanic individuals, and black individuals get included.
Objectives
The main objective of this essay assignment help is to have effective strategies to make the health education program successful. The strategies thereby would be-
• Establishing managerial and support systems in the societal structure
• Offering appropriate health and mental health services for people with asthma
• Offering asthma education with a proper awareness program (Backman et al. 2019)
• Providing a healthy environment to make it safe to not to trigger asthma
• Suggestion for physical education and activity to reduce the chances of the attack
• Proper coordination between all the stakeholders of the society to make it acknowledged by everyone
Delivery Strategies
In order to meet the aim and objective of the health promotion program, the program adopts EXHALE strategies for controlling asthma which eventually can Educate for asthma self-management, eXtinguishing secondhand smoke and smoking. It even confirms Home visits to trigger reduction as well as self-management education to Achieve proper asthma guideline-based medical management to confirm proper Linkage to co-ordinate with care across the setting with a special focus on effective Environment policies or practice to reduce at work, outdoors, or indoor asthma triggers (AAFA, 2022).
Initiating community health, the health program would accommodate the promotion of updated guidelines as per caregivers, patients, and clinicians. It is further been objectified that the promotion of guideline-based asthma care for referred communities or groups gets accommodated in the process (Danvers, Lo, & Gaillard, 2020). Communication with community health workers for reducing asthma triggers at home is important to comprehend. Further launching three national awareness campaigns for lung infections like flu to impact on asthma, controlling symptoms, and use of asthma inhalers and allergic asthma for children are important strategies to include. Most importantly the community health program needs to take care of developing education with effective resources to make the community health promotion program successful to protect the community or society free from such types of issues.
For delivering strategies, proper strategy development is an important consideration to make the pre-planning aspect effective. In the referred strategy delivery the program has taken the help of Asthma Prevention Management And Treatment Communities Approaches For New Millennium and Two National Asthma Education And Prevention Programs (CDC, 2022). 8 interactive components are even accommodated to coordinate the health program.
Strategy development is the pre-planning and planning stage where a strategy implementation is most important to make the health promotions program successful while proper execution. In order to serve the referred communities who are directly involved with the entire concern, the health promotion practitioners need to adopt proper implementation strategies which need a team effort to involve parents, students, medical staff and faculty, medical administrators, social administrators, etc can be used for developing the plan to address asthma for a particular society to make the program tailored as per the need. Such narrowing down can be even helpful to make the implementation or execution successful as every strategy might not be feasible or appropriate for every society. Hence it is important for the social administrator as well as promotion practitioners and medical administrators to determine which strategies can have the highest priority as per the need of the particular society and can have the support of available resources (CDC, 2022). The society and the medical administrator wherever possible initially need to focus on asthma programs to be conducted in society as much as possible accommodating all stakeholders to get rid of emergency situations or hospitalization. As research conveys that residents, minority populations, and low-income experiences higher emergency and hospitalization as well as death than the general population thereby promotion practitioners with the help of social administrators need to confirm if such type of scenario is involved for this particular health promotion program in that area.
Specific Strategies
1. Establish management and support system for an asthma-friendly society - for proper implementation of this particular strategy, it is very important for the promotion practitioners to identify existing for that area as well as resources to meet the needs with proper cultivation of potential barriers. The promotion practitioners would be responsible for proper coordination regarding asthma activities in the area. He even needs to share coordination with the local administrator and health administrator to confirm if asthma coordination can better be integrated with other types of activities (CDC, 2022). It would be better for the promotion practitioners to share the strategies with District Health Council to get help as per need. It eventually helps him to better convey asthma management in society with all support of the health department considering it a higher priority. He can even opt for the implementation or development of written policies and procedures regarding asthma education as well as management to promote the program which is language and culturally appropriate. He is responsible to cultivate recent records of that particular area to be well assured about the need of that particular community. Conducting a survey can even help him to be particular about every individual to use that regular data in health promotion programs for further betterment. The use of individualized education plans with physical activity can help him to spread awareness or acknowledgment in society to confirm support as per need (Isik, Fredland, & Freysteinson, 2019). It will be better for him to take the help of administrative support to have better trust or loyalty in the society which eventually can help in promoting communication with the society stakeholders to confirm the better provision of care. Availability of private, state or federal funding needs to collect to initiate the success of the program.
2. Provide effective health Services for the community with asthma - accommodating a written asthma action plan for all people with asthma can help to accelerate the success of the program. The plan however needs to be developed by the primary care provider to provide it to the parents most importantly. It even needs to include emergency contact information, environmental triggers, peak flow, monitoring medication, individualized emergency protocol, etc (Chen et al. 2019). Promotion practitioners, however, are responsible to share the plan with appropriate people and medical staff to abide by the family educational rights and privacy act guidelines to get parental permission. It is important for the promotion practitioners to ensure that everyone can have immediate access to medication as prescribed by the physician with the approval of the parents. It is important to use standard emergency protocol for the endangered community in respiratory distress if they are left from an asthma action plan. The promotion practitioners are liable to ensure case management as per the database to provide a full-time registered nurse for an emergency situation as well as proper access to consulting physicians. Proper coordination among all the stakeholders is most important to make the delivery of the promotion program successful (George, 2018).
3. Provide awareness programs and asthma education for people - it is important to ensure that all people with asthma can have education regarding asthma basics, emergency response, and asthma management for which it is important that parents are encouraged in participation of the program. Integration of awareness as well as health education to endangered as well as other people to make them prepare for emergency situations. Assistance needs to be provided for cessation programs as well as smoking prevention specifically for the students.
4. Provide a healthy and safe environment for reducing asthma triggers - promotion practitioners need to convey to society that tobacco is prohibited in all media for all the time (Cicutto et al. 2020). He is even responsible to make people acknowledge about prevention of indoor air quality problems by eliminating or reducing allergenic including tobacco smoke, debris, and dust from the construction as these trigger asthma. The use of Integrated Past Management Techniques for controlling pests can be effective.
5. Offering safe, enjoyable physical education as well as activity opportunities - promotion practitioners need to encourage full participation in physical activities specifically among children as well as modified activities for other endangered people like pregnant women, etc. Proper access to preventive medications before activity and emergency medication immediately needs to be comprehended.
6. Better managing asthma symptoms - education support with proper involvement of all family members can help the promotion practitioner to convey the main aspect of the entire asthma health education program to everyone to fight with the issue from a better position. Cooperation or partnership with local community programs can help the promotion practitioners to reach the vast range of society to confirm a wide grasp of the health education program. Arranging seminars, and awareness through social media, print media, and every possible way can be adopted to make the program successful as much as possible (McClure et al. 2018).
Evaluation plan
Evaluation of the health promotion program is important to confirm the success or failure of the respective program. In order to confirm the same, the promotion practitioner with his team would access perceived health status for 3 months to get an idea about healthy behaviors and changes the society has accommodated through the health promotion program. Feedback-giving programs even can be arranged to understand if the taken policy or awareness seminars served the purpose of the same. By making a comparison between initial data to collected data by every 3 months the success or failure of the health promotion program can best be evaluated. The evaluation plan would surely accommodate the purpose of the evaluation, evaluation questions, and criteria along with time table and work plan to collect data in an effective manner. Such type of inclusion can be much helpful for the health promotion program to be evaluated in a proper way.
Conclusion
The paper has confirmed that asthma can even be life-threatening though it is either ignored or neglected in the societal structure which eventually increases the number of severity or death of asthma. Thereby the health promotion program is been formulated to prevent asthma for which the discussed 6 main strategies are establishing a management and support system for a friendly environment, offering appropriate health and mental health services for endangered people, offering asthma education and awareness program for everyone, offering a safe and healthy environment to reduce asthma triggers, offering safe, enjoyable, physical education and opportunities for the community, effective communication, coordination, and cooperation among all the stakeholders. Promotion practitioners are seen as the main responsible person to execute all the strategies in a better way where evaluation plan is much helpful to confirm success or failure for him.
References
.png)
PUBH6006 Community Health and Disease Prevention Assignment Sample
ASSESSMENT BRIEF
Learning Outcomes
This assessment addresses the following learning outcomes:
1. Examine health promotion principle and strategies.
2. Apply concepts of community capacity building and empowerment
3. Integrate health promotion theories and public health frameworks into practice
4. Demonstrate clear and assertive communication across a range of settings and situations
Instructions
Review one existing community-based health promotion program provided by your lecturer. Then use the assessment template to develop a report drawn from your critical analysis and applying theory into practice. The list of health promotion programs and the assessment template will be provided separately.
1. Critically explain the target group of the chosen program in the following topics based on the evidence derived from the chosen program. Use creditable evidence to support you point of view.
• Explain the target population of the chosen program in the context of community health.
• Explain the importance and significance of this prevention among the target population.
2. Use the following topics to critically analyse the appropriateness of the chosen program. Support your point of view with the evidence derived from the chosen program and creditable evidence.
• Aims and level of disease prevention of your chosen program.
• Health promotion strategies (Ottawa Charter strategies) that had been applied to the chosen program.
• Health promotion activities/interventions that had been incorporated into the chosen program such as lifestyle change program, health education session, screening test etc.
• Community capacity building and empowerment strategies (Laverack’s ladder) that had
been applied to chosen program.
• Main communication channels used in the chosen program.
Solution
REVIEW OF CHECK.PROTECT.CONNECT PROGRAMME
Introduction
Lung cancer has become a burning health concern in modern times due to the poor lifestyle quality of people and the rapid increase in addiction to cigarettes. Symptoms of lung diseases are difficult to understand, and people often avoid them. Check.protect.connect provides an opportunity for people to assess their lung health condition. This study focuses on analysing the health promotion intervention considered under Check.Protect.Connect program based on the Ottawa charter strategies. It includes a description of the aim of this program as well as the targeted population. Based on a conceptual framework, it evaluated the concept of community empowerment considered under this program.
Target population
Community health issues addressed by Check. Protect. Connect program are lung diseases and lung cancer. This program focuses on increasing awareness among the community regarding the symptoms of lung diseases. The targeted population of this program is not specific to age groups as this program tagged people who are suffering from lung diseases or people who are on the verge of developing acute lung disease or lung cancer (Lung Foundation Australia, 2021). This program targets Australia's population for making them access help for their lung diseases at the right time.
Lung cancer is the leading cause of death worldwide, and in the year 2012, lung cancer became the cause of death for 1.6 million people. As suggested by Parker et al. (2017) Severity of death due to lung cancer increases as per increase in age. The premature death, disability, and loss of productivity due to lung cancer cost $895 million in the year 2017. Thus it becomes necessary to prevent the severity of lung cancer through early diagnosis. As mentioned by Clark et al. (2020), online screening programs allow individuals to access necessary information for understanding symptoms of lung diseases. Lung cancer prevention is necessary for maintaining the wellbeing of individuals as well as increasing awareness regarding the health consequences associated with poor lung health.
Conceptual Framework of a Community-Based Program
Aim
Check.protect.connect program is developed by Lung Foundation Australia, and from the year 1990, this organization is promoting awareness regarding lung diseases among people (LungFoundationAustralia, 2021). This program developed by this foundation aims to increase awareness among people regarding lung diseases and their symptoms as well as the providing opportunity for equality in care for treating and diagnosing lung diseases.
Level of prevention and approach applied.
This program focuses on preventing the diversity of lung disease through increased awareness and engaging with people who are suffering from lung diseases. Making people aware of the necessary measures for maintaining good health of lungs is the primary approach for prevention considered under the program. The activities of this program are divided into three sections, including Check, protect and connect. In the check section, a checklist is provided to the user that allows the user to identify lung diseases (LungFoundationAustralia, 2021). On the other hand, in the protection section, this program allows users access to advice regarding immunization and areas about health concerns needed to be communicated with the health professionals. Whereas in the connecting section, this program means regular communication with people suffering from lung diseases to ensure needed care and support. Health literacy is the approach applied in this program. As stated by Nehemiah and Reinke (2020), health literature allows increasing the capacity of individuals to understand basic health information. Based on their approaches, the support services of the program include communication with respiratory care nurses, communication with lung cancer support nurses, and other lung disease support groups. Further support for regular exercises for people having serious lung conditions also falls under the service provided under this program.
Explanation of health promotion strategies through Ottawa charter strategies
Ottawa charter health has been developed for achieving health promotion for the areas mentioned by the World health organization (WHO) for the betterment of community health. As per this charter, essential resources of good health include peace and shelter as well as education. Further stability income, availability of resources, and equity also fall under the essential resources as per the charter (Betterhealth, 2021). Strategies for health promotion mentioned under this charter include advocacy, enabling, and mediating. Advocacy approaches of health promotion focus on favourable conditions in terms of environment, cultural and social equity, and economic stability.
On the other hand, enabling a focus on ensuring equality in health services through a supportive environment. Whereas meditating focuses on prerequisite the prospects of health that cannot be addressed by the health sector alone. This strategy ensures coordination of better health service providers and the government for the delivery of health care aids. Based on these strategies, promotions activities under Check.protect.connect programs can be evaluated. The advocacy focuses on enhancing people regarding the right care, which is done through the check stage of this programmer.
On the other hand, enabling people to avail the right facilities within protecting strategy of this program where people are provided an opportunity to communicate with health service providers to access aid. On the other hand, mediating focuses on maintaining coordination which is included under the connect stage of health promotion under this program. Ottawa charter focuses on priorities of health for delivering successful health promotion (Betterhealth, 2021). These areas include building public health policy, creating a supportive environment, strengthening community-based activities as well as developing personal skills, and on the other hand, reorienting health services and moving into a healthy future fall under prioritisation areas under the charter. These areas are considered under the Check, protect, connect program. This program focuses on enhancing public awareness and allowing people to access the required assistance to cope with lung diseases. Further, to avoid issues due to lack of support services to individuals diagnosed with lung diseases and cancer through the science strategies, this program allows supportive aid to people.
Analysis of health promotion activities
The health promotion activities considered under the Check, protect, connect program are based on increasing health literacy and bringing positive lifestyle changes. Health promotion activities considered under the program falls under the criteria of health education and lifestyle change. As opined by Pizon (2019), health education allows people to identify which habits are good and bad for health. Health education allows improving health awareness among people and reducing risk behaviors. Check, protect, connect programs focus on increasing health awareness among people regarding maintaining a healthy lifestyle for avoiding lung diseases. The services provided under the program include special services for users with lung cancer. The other support service provides an expert opinion regarding health conditions and allows users to identify the symptoms of lung disease. As per the views of Haber (2019), health awareness regarding the activities that lead to health wellbeing provides an opportunity for healthy aging. The severity of lung disease in spread the overall age groups, thus guiding people for bringing healthy changes and identification of symptoms at the right time fall under the primary health promotion activities of this program. Health promotion activities considered under this program for best assignment help, focus on improving lifestyle quality of service users for reducing occurrence of lung diseases.
Concept of community empowerment
The strategies considered under Check, protect, and connect program focus on sustaining individuals' awareness of lung diseases. Based on Lavarack’s ladder, this community empowerment made through the strategies considered under the program can be defined. The primary motive of Lavarack’s ladder is to increase community-based interaction that leads to community empowerment. In the considered health promotion program, lavarack’s ladder is applied for establishing interaction between health professionals and people for making them understand that the symptoms of lung diseases and healthy lifestyle need for prohibiting lung diseases. As mentioned by Starns(2019), equality is care facilities that allow delivery services equally to individuals. This program also focuses on maintaining equality by ensuring accessibility of health assistance services to users.
In community programs, communication channels play a vital role in understanding communication needs. As mentioned by Swanwick & McKimm (2017), communication allows understanding the needs based on the need for health interventions that can be further developed. In the Check.Protect.Connect program the service users are communicated through online platforms as well as media platforms. The media platform is utilized for making users aware of the changes in services, and the online platform for making people access the services. Based on the forms filled up through online platforms, different services are provided to users as per their health needs. Online platforms allow better engagement with service users. Online platform provides opportunity to engaging with large target group.
Conclusion
Thus it can be concluded that the Check, protect, connect program focus on maintaining user interaction through online communication platforms. This program includes advocacy, enabling, and mediation of an approach to understanding the risk behaviours that lead to lung diseases. This program allows people to understand the symptoms, whether they have any lung disease or not. Further, this program ensures advocacy that helps to rescue lung cancer which has been a burning health concern. This program includes advocacy as well as focus on enhancing health care policy as well as assistance by ensuring support for people dealing with lung diseases.
References
.png)
EBP107 Evidence-Based Practice Assignment Sample
Instructions:
Students are required to conduct an evaluation of one journal article in an essay format. The article may be the selected one used in Assessment 2 Article Summary task. Alternatively, you may choose to select an article of your choice from the range of research articles supplied for the previous Assessment 2 assignment.
This task requires using one of the critical appraisal tools supplied from a link below. Choose an appraisal tool that fits the chosen article to evaluation.
• CASP. (n.d.). CASP Checklists. Retrieved from https://casp-uk.net/casp-tools-checklists/
• Centre for Evidence-Based Medicine (CEBM). (2014). Critical Appraisal Tools. Retrieved from
https://www.cebm.net/2014/06/critical-appraisal/
• Equator Network.(n.d.). Reporting guidelines for main study types. Retrievedfrom
http://www.equator-network.org/
• Joanna Briggs Institute (n.d). Critical appraisal tools. Retrieved from
https://jbi.global/critical-appraisal-tools
Essay Format:
The article evaluation must be presented in an essay format, with an introduction, body and conclusion.
Introduction:
The introduction must introduce the article, including proper referencing of the article, and a discussion about why you chose that article to evaluate.
Body:
In the body of your essay you must:
1. Use the critical appraisal tool you have chosen to evaluate all the sections of the research study, including the title, abstract and declarations.
2. Throughout the body of your essay you are to refer to the chosen critical appraisal tool and use additional references to support your evaluation. Subheadings may be used.
3.. Provide a referenced definition of Evidence Based Practice (EBP), and a recommendation as to how well the findings from this study may be incorporated into EBP. Give reasons and offer evidence to support your evaluation.
Conclusion:
A brief discussion of the overall quality of the study with reference to the strengths and weaknesses as outlined in the body of the essay.
Referencing: It is essential that you use appropriate APA style for citing and referencing research. Please see more information on referencing here: https://library.torrens.edu.au/academicskills/apa/tool
Word count: Please include the word count - excluding in-text citations and reference list at the end of the assessment. Please adhere to the word count, if you exceed 1,500 words (+10%), the excess may not be graded.
Appendix: Include a copy of the completed critical appraisal tool as an appendix.
Solution
Introduction
This study aims to conduct a critical evaluation of a journal through the assimilation of the CASP tool. Long et al., (2021) in this comment that CASP is a potent tool that is employed predominantly to assess the limitations and soundness of qualitative research methodologies. In this particular context, a journal is integrated that identified whether the consumption of eggs and cholesterol impacts the cardiovascular health of an individual. This particular article has been chosen here to know whether the consumption of egg is dangerous for the people having cardiovascular disease. The essay aims to bifurcate the legitimacy and transparency of the study and its applied method critically for best assignment help.
Discussion
Employment of critical appraisal tool
To evaluate the essay critically CASP checklist has been incorporated as it embodies some prompt questions to assist the research study effectively. After going through the journal systematically, it can be said that the study from the very beginning made it absolutely clear whether the consumption of eggs and intake of cholesterol plays a vital role in the cardiovascular health of an individual. Additionally, the aims of the study clearly state that it aims to associate the study with cholesterol intake and morality rate from CVD in the US population.
In this particular study, the cohort is recruited in a coherent manner. The NIH-AARP study was a vehement perspective cohort that was integrated between October1995-may1996 when a questionnaire was forwarded to around 3.5 million AARP (Zhuang et al., 2021). The final analytic cohort consisted of around 500,000 participants and this particular study is assimilated as per the strengthening of the conducting of observational inculcation in epidemiology statement. Additionally, through answers to study-oriented mailing, the “US postal service national of address database”, and direct conversation with cohort members, all the participants were scrutinized for the changes in their address.
The researchers integrated data of 521,120 participants from the NIH AARP diet and health study while integrating a median follow-up of over 15 years to examine the impact of egg and cholesterol intake with specific morality. However, since it is a "randomized controlled trial with random modeling," the approximation cannot be considered to be entirely accurate.
The result demonstrated around 129,328 deaths including 38,747 deaths during the integration of median follow-up of over 15 years. It demonstrated that both whole egg and cholesterol intake were positively associates with all-cause, CVD, and cancer mortality. Additionally, a multivariable adjustment model was integrated to minimize the bias to a comprehensive extent.
It was found that the additional half of a whole egg daily was around 1.07 for cancer, 1.07 for CVD, and 1.07 for all-cause mortality (Zhuang et al., 2021). Mathematically speaking if an individual consumes 300 mg of dietary cholesterol maximized around 19 percent, 16 percent, and 24 percent mortality rate associated with all-cause, CVD, and cancer.
The methodology has effectively integrated multivariable models and meditation models to individually examine the impact of cholesterol and egg simultaneously. In both cases, the statistical analysis puts forward a positive correlation of morality rate with consumption of eggs and dietary cholesterol. However, the approximation cannot be regarded as being truly accurate nevertheless, as it is a "randomized controlled trial with random modeling". Here, the confidence intervals give a "range of values" rather than a "single value" for the forecast, allowing one to assess the degree to which the conclusions of the study may be believed.
The follow-up has been maneuvered for more than 15 years (Zhuang et al., 2021). It enables the researchers enough time to establish the proficiency of their findings.
The result states that the intake of eggs and dietary cholesterol are closely intertwined with CVD, all-cause, and cancer mortality. Hence, all individuals must limit their cholesterol intake while incorporating egg white instead of whole eggs to lead a healthy life. In terms of the result, the table of Baseline Characteristics and All-cause Mortality has been mentioned properly. Additionally, the abbreviations and table headings were noted to retrieve accurate outcomes. The research examined and analyzed the relationship between the “consumption of eggs and cholesterol”, particularly in terms of morality from various causes among 521,120 participants with a “mean follow-up” of 16 years. The results are quite precise as the study utilized “cause-specific hazard models” for considering competing risks to calculate hazard ratios as well as 95% confidence intervals of “all-cause” and “cause-specific” mortality based on different categories of consuming egg and cholesterol. However, as it is a “randomized controlled trial with random modeling”, the approximation cannot be considered genuinely accurate. A “range of values” is provided here by the confidence intervals instead of a “single value” for the forecast, hence allowing to determine how much the research findings can be trusted.
The results of this study are identified to fit with other accessible evidence. It is so as the ultimate outcomes have demonstrated consistency with joint research of “6 prospective US cohorts”. The study has finally reported that consumption of an additional half egg/day is closely associated with an 8%, 6%, and 8% higher risk of CVD mortality, incident CVD, and all-cause mortality. Meanwhile, a similar pattern has been reported by the study for the association between consuming non-fried and fried eggs while observing an inverse alliance between consuming “egg-white substitute” with mortality. Therefore, underscoring the negative impact of “egg yolk” and “cholesterol” in premature deaths. The research has explained the clinical relevance well and it has been observed that the study would not exceed a statistical significance. Additionally, the “internal validity” of this research was high as it identified and presented the entire structure in an appropriate manner. The protocols were analyzed and approved despite the actuality that all the collected data have a significant value. However, the research is not limited to any particular population and can be applied to the local population. Additionally, the study is that its external validity failed to meet the standard level, though it has an enormous impact on the health and longevity of human beings. Therefore, it can be used for acknowledging and reducing risks associated with diet and lifestyle.
Critical evaluation of the appropriateness of the chosen cohort study
In this study, 521,120 participants were involved from all across the United States. The study has finally reported that consumption of an additional half egg/day can cause a higher risk of CVD mortality, cancer, and all-cause mortality. As stated by Zhuang et al., (2021), it is important to limit “cholesterol intake” and replace whole eggs with egg whites or other alternative sources of protein to facilitate “cardiovascular health” and “long-term survival”. On the other hand, Zhong et al., (2019) have included and analyzed 29 615 participants to shed light on the associations of egg consumption and dietary cholesterol with the “incident cardiovascular disease” and “mortality”. However, the result showed that a higher consumption rate of “dietary cholesterol” can increase the risk of incident CVD as well as all-cause mortality among US adults, particularly in a dose-response manner. Additionally, Panizza et al., (2018) have created “The Healthy Eating Index-2015” for assessing the accordance of dietary intake with the “Dietary Guidelines for Americans (DGA) 2015–2020”. The result showed that there is an inverse association between high “HEI-2015 scores” and “risk of mortality” from CVD, cancer, and all-cause for both men and women. Moreover, Mazidi et al., (2019) have identified that there is no direct link between total as well as CHD mortality with egg intake in men and women. The study has also resulted that egg intake has a “reverse association” with stroke mortality among men, though it is not significant among women.
Evidence-based practice
EBP is a procedure employed to review, examine and transcribe the latest scientific research. The key goal of this particular process is to integrate the best possible research into medical and clinical practices. It enables medical professionals to integrate informed decisions (do Vale et al., 2021).
The study integrates a positive correlation between mortality from all-cause, CVD, and cancer, and increased in-take cholesterol. However, they completely discarded the fact of the difference between good cholesterol and bad cholesterol. It integrated a hypothesis and considered cholesterol derived from the egg as LDL. On the other hand, the study also completely discarded that the majority of the cholesterol in our body is made by the liver itself. Hence, a series of discrepancies is prevalent in the present study. Numerous reports suggest that the cholesterol derived from eggs is not LDL. On the other hand, the liver is being stimulated to formulate cholesterol by saturated and Trans fat in our diet which acts as a prerequisite for the body (Li et al., 2020). Additionally, the nutrients present in Eggs such as Lutein, zeaxanthin, choline, and others work wonders for the eye and brain. However, it cannot be denied that the fried egg puts forward a positive correlation with bladder cancer. The risk is mitigated automatically when it is consumed or boiled (Chen et al., 2021). Therefore, one egg a day can be a belling in disguise to meet the prerequisites of protein, vitamins, and good cholesterol. However, people suffering from cardiovascular disease must take expert opinion and consumes it in modulation. It is also recommended that the egg must be consumed boiled rather than fried to mitigate the chances of cancer.
Conclusion
In this particular situation, a journal has been included that determined whether egg and cholesterol consumption affect a person's cardiovascular health. Since it is a "randomized controlled trial with random modeling," the approximation cannot be considered to be entirely accurate. However, the researchers integrated data of 521,120 participants who have been followed up of over 15 years to examine the impact of egg and cholesterol intake with specific morality, hence, the result of the study clearly shows a strong temporal succession between the research cohort and the result which shows the reliability of the research outcomes. However, since it is a "randomized controlled trial with random modeling," the approximation cannot be considered to be entirely accurate.
The confidence intervals in this case provide a "range of values" rather than a "single value" for the forecast, enabling one to judge how much the study's findings may be trusted. Hence, the recommendation has been modified after the identification of the gap in the study.
References
.png)
CAM529 Introduction to Public Health Assignment Sample
Task description
Background:
Cardiovascular disease is considered by the World Health Organisation to be the “world’s number one killer.” This group of diseases causes considerable morbidity and mortality worldwide, and greater than 75% of cardiovascular disease deaths occur in low and middle-income countries
Task:
You are to write an essay describing the global health problem of cardiovascular disease. You should consider how the epidemiology of heart disease differs in low, middle and high- income countries, and the reasons for this. Imagine that you are working for a regional office of the World Health Organisation
You can choose which WHO regional area you wish to focus on. You should then search for and interrogate the literature on current public health challenges and responses to cardiovascular disease for your chosen region and use this information to make recommendations for future action.
Your essay paper should be structured as follows:
• Introduction: Introduce the topic and define the scope of your paper.
• Background: Include the most recent data to illustrate the public health problem in your region, and describe how the problem differs within and between countries in your region. Discuss the determinants of health that are relevant to this issue and explain how they contribute to disease burden.
• Public Health Response: Based on your reading of the literature, describe the current public health policy and strategy responses to this issue in your defined geographical region. Critique this response – identify strengths, weaknesses and gaps, as well as opportunities in relation to the current response. Consider public health approaches that you believe will reap the greatest population health gains. Support your arguments with reference to relevant scholarly literature.
• Recommendations: Based on your critique of the current public health response, provide three policy recommendations for improving the disease burden of cardiovascular disease in your region of choice, and identify the governing bodies that would be responsible for enacting these recommendations.
Task length
The essay should be approximately 3000 words (including references, tables and figures). A word count within 10% of this is considered acceptable.
Solution
Introduction:
It is to be noted that “Cardiovascular Diseases” are the number one killer disease in the world. Globally, an estimated 18 million people had died suffering from cardiovascular disease and amongst all these deaths, more than 85.2% deaths had been due to “stroke” and “heart attack” (Bansal, 2020). Over three-quarters of cardiovascular deaths occur within low and middle-income countries. Amongst 17 million premature deaths in 2019, more than 37% of the deaths had been caused by CVDs (Mehra et al., 2020). The essay discusses the various aspects of cardiovascular diseases and a discussion entailing how heart disease differs in low, middle, and high-income countries (Fuchs and Whelton, 2020). The WHO region that has been taken under consideration in this paper is “South-East Asia” (Peltzer and Pengpid, 2018). The various public health challenges and responses towards “Cardiovascular diseases” for the chosen region would be carried out and some relevant and suitable recommendations would be made for future actions (Dehghan et al., 2018). It is needless to mention that it is of utmost importance to detect cardiovascular diseases at the earliest so as to manage, counsel, and discover effective cures and medicines for the disease (Thomas et al., 2018). The scope of the paper is that it would help future epidemiologists to find the spread, and measures of Cardiovascular diseases within the various high, medium, and low-income countries in South-Eastern Asia for assignment help.
Background:
Heart diseases account for more than 33% of all deaths take place in the South East Asian region and as per reports, cardiovascular diseases are responsible for more than 4 million people every year (Oliva, 2019). Within the region some of the majorly identified causes of cardiovascular diseases (Shafiq et al., 2018). In addition to this, the high blood pressure, as well as unhealthy diets, air pollutions, and so on, are some of the most important risk factors for cardiovascular diseases in the South East Asian regions and they account for more than 18 percent of the total number of deaths and 28 percent of the cardiovascular-related deaths (Jankowski et al., 2021). According to the study by Zhao (2021), amongst all deaths from CVDs, 39% percent of deaths in Southeast Asia are caused by Ischemic heart attacks, 49% percent of deaths are caused by Stroke, and 12 percent of deaths are caused by other cardiovascular diseases (Zhao, 2021).
Low income countries: Bangladesh:
Bangladesh is one of the low income countries of South-east Asia and a recent study from the rural Bangladesh has demonstrated that a there had been drastic increment in the cases of cardiovascular diseases between 2010 to 2019. The age-oriented cardiovascular diseases had increased by 30 times (Islam et al., 2016). Also, it can be said that Bangladesh has exhibited some prominent increment in the prevalence of some non-communicable chronic diseases and the related ates of mortality and morbidity in the previous few years (Islam et al., 2016). Some of the major health determinants pertaining to the prevalence of cardiovascular diseases in Bangladesh include hypertension, diabetes, body-mas index, raised blood pressure, education and so on. As Bangladesh has experienced some rapid urbanization within the last few decades and also exhibited fast economic growth and thus has recently emerged as “a developing nation” (Sharif et al., 2021). As a result of this increased urbanization and growth, there is an increasing concern about further risks of chronic diseases due to the habits of people to adopt sedentary lifestyles (Barua et al., 2018). Bangladesh has also undergone changed food habits and increased inclination of young and middle aged people towards processed foods and inconsistent means and reduced physical activities (Islam et al., 2016). It is to be noted that poor lifestyles are being increasingly adopted by the people of Bangladesh, and as a result, more and more people have been suffering from Coronary Heart Diseases and renal failure than ever before (Hahn et al., 2021). Also, within Bangladesh, the males, unmarried people, the non-slum urban people and the non-Muslims tend to greater possibilities towards the risks of cardiovascular diseases (Barua et al., 2018). In addition to this, according to many studies, the Cardiovascular disease risks had been seen to be conversely proportional to the level of education amongst the males and females and Bangladeshis. For the people having more than 1 years of education, the chances for them to suffer from elevated cardiovascular disease risks is less than 10% (Sharif et al., 2021). Thus, education can be an effective way to prevent and control the risks of CVD within the country.
Middle-income countries: India
In the of the Southeast Asian regions, India is a developing nation with middle-income, and in this country, hypertension, stress-related brain activities, and so on have been reported as some of the most potential factors attributing to cardiovascular deaths (Peltzer and Pengpid, 2018). In the 21st century, Cardiovascular diseases had been one of the most significant causes of mortality in India (Geldsetzer et al., 2018). As compared to the people of Europe, the Indians are affected by cardiovascular diseases 10 years earlier and mostly during the most productive period of their lives. In India, amongst all deaths caused by cardiovascular diseases, 52% are middle-aged. It is to be noted that the most prominent health determinants pertaining to cardiovascular diseases in India is include age, gender, unhealthy food habits, sedentary lifestyles, consumption of tobacco and alcohol abuse.
Moreover, the case of fatality that is attributable to cardiovascular diseases within the middle-income countries like India is significantly higher than high income countries (Kundu and Kundu, 2022). As estimated by the World Health Organization, with the present burden of cardiovascular diseases in India, the nation might loose more than $230 billion from productivity losses and expenditure within the healthcare in the coming decade. In India, the high propensity to develop Cardiovascular diseases can be attributed to various biological mechanisms, various social determinants and other interactions (Nambiar et al., 2020). Migrant Asian Indians have three-times greater prevalence of coronary artery diseases within the rural parts of the country (Kundu and Kundu, 2022). Moreover, the prevalence of Coronary artery diseases within Indians is more than 22 percent for the diabetic patients and 11 percent for the non-diabetic ones. The coronary artery disease prevalence within the rural parts of the nation is more or less 50 percent than within the urban population (Nambiar et al., 2020). Therefore, in order to address the significant burden requires a thorough understanding of all sociological and biological determinants and the complex dynamics underlying the various interactions as well.
High-income countries: Thailand
As per the latest World Health Organization data for 2018, cardiovascular diseases including coronary heart diseases in Thailand has reached more than 60,372 which is equivalent to 12.35% of the total deaths in the country (Juntarawijit and Juntarawijit, 2020). The “age adjusted Death Rate” of the country as per WHO report is approximately 63.10 per 100,000 of population ranks the country #157 in the world. In this country, the main health determinants relevant to cardiovascular diseases include “high blood pressure levels”, “high cholesterol levels”, “diabetes”, smoking, and so on (Juntarawijit and Juntarawijit, 2020). In the last decade, there had been a drastic increase in various chronic diseases within Thailand and Cardiovascular diseases and coronary artery diseases had a significant rise. In the year 2019, in Thailand there had been more than 350 thousand patients undergoing “ischemic heart disease” (Jensen et al., 2019). In that same year, the highest number of patients suffering from Cardiovascular diseases was from Bangkok and there were nearly 48 thousand patients. In the last decade, the number of Thai people suffering and dying from CVD including coronary heart diseases had been increasing in a drastic manner and had been considered to be one of the major causes of deaths in Thailand (Gheewala et al., 2019). The most potential factors that can be attributed to these diseases are unhealthy food habits, and the drastically changing eating behaviours of the people. The Thai people often eat high fat content and high carbohydrate content foods and also they barely exercise but exhibit high levels of stress. In the increasing rates of cardiovascular diseases in Thailand, genetics also play a significant role (Hahn et al., 2021). Apart from that, hypertension, high cholesterol, increasing rates of obesity, smoking and adoption of sedentary life styles are also some of the major factors contributing to the increasing cardiovascular disease rates in Thailand (Krittayaphong et al., 2019).
Public Health Responses within the region
At present, the South Asian tends to account for one-fourth of the total world population, and yet it already claims nearly 60 percent of the worldwide burden of heart diseases (Hahn et al., 2021). It is to be noted that the burden of cardiovascular diseases ion would continue to increase in a drastic manner within the region of Southeast Asia in the future few decades. Substantial public health achievements had been made in the prevention of cardiovascular diseases and strokes; however, they are not sufficient to prevent or reverse the epidemic (Zhao, 2021). Public health services societies by guaranteeing conditions of life where the people can be healthy by addressing 3 major functions, namely, assessments, policy development, and assurance (Thomas et al., 2018). Fruitful achievements within these areas include effective assessment, policy development, and assurance (Peltzer and Pengpid, 2018). For many decades, Southeast Asian public health agencies and epidemiology researcher’s has gathered data on cardiovascular diseases and had carried out research on the ways to measure and prevent them. Despite the persistence of some crucial gaps, the collected information tends to provide a great evidence-base for effective decision-making by public health (Oliva, 2019). Moreover, a wealth of various policies had been developed based on the gathered knowledge and some policies had been implemented in an effective manner but await broader and more intensive applications in order to gain the optimum impact (Dehghan et al., 2018). The others had yet to be acted on. The evaluation of all these policies needs the implementation on an optimum scale and enough resources for evaluation. It is important to note that assurance is evaluated by the level at which the society is protected from the cardiovascular diseases and strokes that can be attained in spite of the latest progress (Dehghan et al., 2018). Therefore, it can be said that the public health agencies can out the recent knowledge for working through a targeted plan of action. However, it is unfortunate to note that most public health agencies are not yet “well-equipped” for these tasks. Within the region of Southeast Asia, this is considered to be further complicated by the provisions of “care split” amongst public and private systems (Shafiq et al., 2018). Primary care services can one of the main contributors to heart and cardiovascular diseases and should be strengthened for realising the actual integration of care for “secondary prevention of cardiovascular diseases”.
However, in the public health response in Southeast Asia, there is a lack of patient participation in the various rehabilitation programs and there is poor adherence to the medication (Fuchs and Whelton, 2020). These are the two main issues associated with the public health responses within south-east Asia and these must be addressed to strengthen the secondary prevention responses for heart diseases. It is to be noted that the evidence-based patient education and empowerment initiatives tend to be lacking all over the region and thus must be prioritized. The uses of technologies might provide scopes within the area. Improving and expanding the registry data coverage is important for understanding the actual views of the disease and informing policies (Fuchs and Whelton, 2020). The data integration via “electronic health records” is lacking at present, however, might contribute to that goal. Strengthening the monitoring of the “secondary prevention goals” within the non-communicable diseases or cardiovascular plans and auditing services, delivery based on the establishment of quality standards, and the patient outcomes must be regarded as high priorities for studying economies for refining the healthcare offerings and assure that the requirements of patients are met (Jankowski et al., 2021).
The gains against cardiovascular diseases, in particular, and the impact of the better interventions are, without a doubt a great news. At the same time, they tend to introduce a new problem. Within high-income countries like Singapore, there are an increasing number of people who are now the supervisors of heart attacks and strokes (Mehra et al., 2020). The more the supervisors the more likely it is that there would be more survivors of heart attacks and the more there will be a recurrence of the diseases. The data sets that describe the prevalence of ischaemic heart diseases and strike certainly tend to tell a story of “long-term growth” (Hahn et al., 2021). Thus, it can be said that an ever-increasing part of the population is considered to have cardiovascular disease and might survive a heart attack or a stroke (Peltzer and Pengpid, 2018). This tends to demand some urgent attention but also tends to represent a realizable opportunity for assuring those individuals get appropriate care. For instance, the fight against tobacco can be considered the most important public health success (Thomas et al., 2018). The prevalence of smoking between 1990 and 2015 has declined in all study economies, minimizing the risks of cardiovascular diseases. During the same period, a considerable increment in the population percentage of those who are obese in the economies (Peltzer and Pengpid, 2018).
It is to be noted that the “WHO south-east Asia regional office” had coordinated the development of “national cardiovascular control programs that focus on secondary prevention of community and primary care settings within the countries like Thailand, Indonesia, and so on. Moreover, the “Global cardiovascular atlas report” of 2011 depicts a list of some “best buys” of some immensely cost-efficient interventions, strategies, and policies for preventing and controlling cardiovascular diseases which can be feasible for the implementation within the middle and low-income nations of the region (Dehghan et al., 2018). These include various effective public health strategies that address various behaviural risk factors like tobacco and the use of alcohol or unhealthy diet practices. Combined with some interventions for secondary preventions like the use of “aspirin, beta-blockers, angiotensin” turning enzyme inhibitors and the lipid lowering therapies, the risks of “recurrent vascular events can be reduced by approximately 75%. It is to be noted that within Southeast Asia, the cardiologist density is decreasing while the need for cardiology is increasing at an incredible rate, especially within the low and middle-income nations (Babatola, 2018). Therefore, cardiologists tend to feel overloaded and frustrated with the trends. In spite of that, the health administrators and the policy makers would need some comprehensive data for considering the aspects for some future planning of the health workforce, provided the rising prevalence of the heart diseases and the requirement for “coordinated care”. This would continue to exert pressure on the health systems (Thomas et al., 2018). The need for balancing the other public health policies must be recognized, but the most significant challenge here is that it is not just about increasing the number of the cardiologists, and even if there are an adequate number of doctors to take care of the elderly population in a more generic manner, many cardiologists would just move out of the “public services” to the private service due to the financial incentive and the flexible workloads (Cheong et al., 2019).
Recommendations:
It is important to note that the World Health Organization demonstrates the public health surveillance as a continuous, and systematic collection as well as analysis of interpretation of various health-associated information required for the planning, implementation, and evaluation of the “public health practices” (Cheong et al., 2019). The most important aspect of policy development for Cardiovascular diseases is that effective data should be collected, analyzed, and should be well-communicated to the stakeholders. The main bodies who would play the prior roles in the policy development include the policy makers, the scientific communities, and the planners of the program along with the medical institutes, the Public health authorities, and the funding agents (Roth et al., 2020).
The most significant feature of an effective action framework for preventuig and reducing Cardiovascular diseases is that the framework should entail the present reality which should briefly summarize the current knowledge of the progressive development of cardiovascular diseases and stroke. A vision of the future that summarises the most favorable situations that should be achieved if the cardiovascular disease hazards are to reverse or arrested. Also, the framework must also consist of a set of strong “intervention approaches” that should include a number of wide approaches that when completely and effectively implemented can help to bring out the transitions to the future healthy people and partnership goals for minimizing the heart diseases and the stroke and the way the 6 intervention approaches could fulfill the various stages of the disease and can facilitate the achievement of these goals. In addition to that, the policy framework must also consist of the target population that indicates the way people can reach the successive intervention approaches (Baddour et al., 2020).
In The Southeast Asian region, the framework for combating the rising urgency of cardiovascular diseases, especially in the low and middle-income countries includes taking action by translating the current knowledge into effective public health actions (Cheong et al., 2019). The policy must have strengthening capacities for transforming the public health agencies with the new and advanced resources and competencies and by expanding strategic partnerships with the high-income countries within the region such as Singapore, and Malaysia in order to sustain and mount those actions (Baddour et al., 2020). Moreover, the policy framework must be efficient enough to evaluate the impact of the actions by monitoring and evaluating the health impact of the interventions (Thomas et al., 2018). The Policy makers and the government bodies within the regions must generate advancing policies that demonstrate the most crucial policy issues and pursue the required preventive actions and research practices to solve those issues and expedite the development of policies (Cheong et al., 2019). The scientific communities and the program planners must also engage in various regional as well as global partnerships by multiplying the resources and by capitalizing on the shared experiences with the others throughout the global communities who have been addressing similar types of challenges.
Conclusion:
The paper has entailed a detailed discussion of the epidemiology of cardiovascular diseases within a chosen WHO region, that is South East Asia and it entails a brief evaluation of the spread of the disease within low, high and middle-income countries and the various measures and preventive actions taken by the region against the epidemic followed some recommendations entailing how the preventive measures, and the controlling policy framework within the region can be strengthened and made more effective. From the study, it can be concluded that in order to develop an effective public health policy within the Southeast Asian region, it is important for the policy makers to communicate the plan to the public at large and to establish some significant awareness and concern about the disease. It can thus be said that a comprehensive and a highly effective public health strategy for the prevention of heart diseases and strokes tend to depend on a broad understanding of the fact that the cardiovascular diseases in the Southeast Asian region tend to threaten the health of mainly the middle aged and the older adults and this can be prevented and controlled by the reversal fo the various acquired behavioral practices such as sedentary lifestyles, unhealthy diets, smoking and so on.
Reference list:
.png)
.png)
.png)
PBHL20007 Cultural Immersion and Lived Experience Assignment Sample
We each come to public health with a set of our own beliefs, assumptions, experiences, judgments, and views that reflect our culture and upbringing, as well as the events of our life. For this assignment, you must think about your own health experiences and the way they have been impacted by your cultural background and the way you think about health and illness. Firstly, think about how your family deal with illness or treat illness condition. Do they use home remedies to treat illness? How do they decide an illness is serious? What are their preferred ways of managing health and illness?
Secondly, compare how your own personal experiences relate to the views and actions of other people in the same community. Is your family in the majority when it comes to dealing with health and illness? Do they act differently to the most people in the community? If they are different, then explain why and how their behaviour was shaped that way which made them different to others in the community.
Thirdly, discuss your own assumptions about health.
Who do you think is responsible for health - the individual involved, the family, the society in which he or she lives, the government, health services or others? To what extent, do you think people should manage their own health? Who should carry the risk associated with disease and illness?
Finally, consider the role that culture and social background play in health and illness.
Discuss the ways this might affect professional practice in public health, including why it is necessary for a public health practitioner to be aware of cultural differences in health and illness.
This is an individual 2000 words reflective assessment. Your reflections to these areas should be supported by evidence from literature, textbooks or other authentic sources. All references must be cited appropriately with a reference list. In drawing on your own experiences, you may use pictures and other creative material to help illustrate your reflections, but these must also be appropriate cited if they are not your own materials. You cannot use materials from google or any internet sources which does not meet academic standards and guidelines.
This reflective practice assessment will be assessed against following criteria.
1. A deep reflection with ability to write clearly following academic coherence
2. Logically draw and analyse personal experiences around health and illness
3. Critically examine and compare the familial and social context of health
4. Succinctly provide evidence-based arguments around different conceptualisation and accountability to health
5. Appropriate grammar, citation, and referencing
Solution
Introduction
In the present times, health issues are becoming more significant as the population and portions of the society are getting affected by illnesses such as diabetes, infectious diseases, HIV, mental health challenges and many more. Nutrition and lack of physical activity led to obesity which can cause many of these diseases. This essay for assignment help will discuss my experience with Bangladesh's approach to health conditions. This will take into account my family's experience in healthcare. This will also compare my experience with society's concepts of health issues and treatments. The role of society and culture in health issues will also be stated. This will help in clarifying the idea about health issues in the society and the people of Bangladesh.
Family's approach to dealing with health conditions
The approach of Family-Focused Healthcare is becoming more popular in contemporary times as health professionals believe that the involvement of the family can help many diseases to get cured faster. Many states and nations are adapting the task of reform in healthcare that seems appropriate considering the various merits of the family perspective. Recently through research, it has been considered by various researchers, healthcare professionals and advocates that family has a profound force on the health of an individual. Every country should support and strengthen its family caregiving programs based on this respective research (Wisconsin Family Impact Seminars, 2022). Although in Bangladesh, I have seen that my family has always been very supportive during my illness and provided the best care that helped me recover faster. The approach of family care is also more cost-effective and focuses on individuals' help in the recovery process. Family members also have a high level of influence on the health habits of each other. The nutrition we get from our food is consumed through a pattern that we learn from childhood. The habit of exercising regularly is also a common habit that we acquire from our family. Family distress is also a common cause of individuals' ability to focus on the negatives only. For example, a person suffering from hypertension who lives alone will not be able to provide proper health care to themselves compared to a man who lives with a family with the same disease. The family also plays a very vital part in relapses of various chronic diseases. Families in Bangladesh are quite dependent on home remedies as various areas are below the poverty line and do not have the resources to visit medical centres. The infant mortality rate is also high as many mothers do not make it to the hospitals or the health care providers during childbirth.
In my family and others around me, I have seen several instances, where social support and stress have helped in decreasing or increasing the family member's likelihood to fall ill. This can happen due to several reasons like a bereavement of a spouse or close family member, the detrimental effect of smoking or alcoholism and many more. Any person who is susceptible to stress can fall ill much faster. Families that face prenatal conflict often have cases of children who are lower than five years with high levels of stress hormone in the blood. Marital distress can also reduce the immune system functioning in many individuals. A family's decisions and beliefs about health care are very important to promote a healthy lifestyle. The chronically ill patient is dependent on the family members' setting of care provided to them which is quite important. Many times,it has been observed that the cohesiveness of a family during the acute stage of an illness generally decreases if the illness remains for a prolonged period. For example, a cancer patient is often seen to have less distress compared to their spouse or family members. Families also need therapy and support when their family members are going through those issues.
.png)
Figure 1: Family’s role in healthcare
Source: (Wisconsin Family Impact Seminars, 2022, para. 4)
Comparison of personal experience with people of the society regarding health issues
I would start with my experience of the pandemic that we had faced in the last two years and yet the world has not recovered. I learned during this period that every year new pandemics emerge that may or may not be as widespread as the Covid-19 virus. This period has taught me that health education and responsible practices in agriculture and society will help in combating such issues in the future (Hossain, 2020, p.1). Another global challenge that I see around me is the pollution and climate change that is leading to the formation of many new diseases. In many societies, economic disparity and the lack of access to healthcare often lead to diseases and high mortality rates. As a society, there is not much contribution that is done to erase such economic disparities even when individuals are seen to be unable to afford health care. I believe there is an equal role between society and the government in the health services that are provided to us. Managing one's health is very important before we start blaming the communities around us or the government.
I do not believe that my family falls under the majority of the society and how they tackle health issues. The main reason which I can attribute to this is lack of resources as most Bangladesh citizens do not have sufficient income to visit healthcare centres. This forces them to surrender to home remedies which are in many cases not helpful. Moreover, the lack of education in many such families leads to a misconception about health issues that further leads to the wrong treatment of the disease. This can only be combated if the government provides a proper health care system and education to all the citizens of the country.
.png)
Figure 2: Bangladesh health care spending shows a significant increase
Source: (TheGlobalEconomy, 2022, para. 2)
Personal assumptions about health
Bangladesh belongs to the category of pluralistic health care system where healthcare is highly decentralised. There are various for-profit companies, international welfare organisations, government schemes and NGOs. This has caused various problems that have caused unequal treatment between various classes in society. Shortage of specialists, clinical equipment and physicians is quite common in the country. There are only 1.07 % of nurses available for 10000 people. The number of physicians per 10,000 people is only 3.06 % (Thelwell & Tashin, 2022). The leading cause of death in the country is non-communicable diseases. These diseases include diabetes, cardiovascular disease, cancer, malnutrition and so on. I have seen that most of the physicians and healthcare centres are only concentrated in the urban areas of the country. The rural hospitals are poorly funded which means there is limited access to healthcare options. The government does not provide sufficient healthcare funding as a citizen has to pay 63.3 per cent of the total cost of the treatments (Thelwell & Tashin, 2022).
According to my research, I have found that Bangladesh has shown remarkable progress in healthcare in the last few decades. Bangladesh strategies include out-of-pocket payments, general revenue taxation and development partners' contributions which include insurance (Fahim et al., 2019, p.2). The problem in this case that has been observed is that 5 million people fall into poverty because of exorbitant health expenditures (Sarker et al., 2022, p.4). Unfortunately, I could not find enough data which supports the out-of-pocket costs that are related to the healthcare expenditures in Dhaka. The sustainable development goal of the country is focused on promoting the well-being of every citizen irrespective of their age. This goal will also focus on the socioeconomic factors and the democracy of the population to see if the OOP has any influence on the health care expenditures of the urban citizens. It is also important to understand that despite the various help provided by the government, one should be careful about the various diseases that are surrounding them. The risk of diseases cannot be single-handedly attributed to the government or the nation. I have observed during the pandemic that there were various cases where the public of the nation was casual enough even when they were provided with all healthcare advisories. This had led to the increase in the spread of the virus. Hence, I strongly believe that it is important to be aware of health oneself too.
Role of society and culture on health and illness
The local perception of disease has been seen to vary from community to society all around Bangladesh. Even though long exposure to illness has not enabled these populations to capture a proper explanation based on the scientific background which can be backed by germ theories. diseases are generally divided into subcategories namely lamani (diarrhoea), pansa (chickenpox), dudher haga (watery white excreta), lunti (measles) sardi or kasi(cough and cold). Even while various health education programs like BRAC provide specialised dissemination about diarrhoeal diseases, it has not helped much with the notions of the villagers (Khan, Bhuiya & Chowdhury, 2022, p.2). Although the villagers are aware of the various health risks associated with taking food without adequately washing their hands or even keeping the food in an open area, it has not brought many changes in their attitude. The dependency on various religious beliefs and the older customs have made these villagers not understand the importance of scientific data that backs the diagnosis of the diseases. Other reasons include workload on the head of the household, where, for example, they are not even aware that the soap is bought after the entire consumption. The poor villagers who do not have the access to simple three meals a day would not buy soap or slab latrines to avoid diseases.
Environmental sanitation according to me is also a very important role that plays part in a healthy lifestyle of a society. In Bangladesh, there is a multifaceted sanitation problem that starts from the basic hygiene requirements like safe drinking water and also prevention of excreta disposal methods. Indiscriminate defecation results in various waterborne and filth diseases including diarrhoea, hepatitis, dysentery, hookworm, and so on. The rural housing setup has no arrangement of proper lighting and ventilation. Most marketplaces and public eateries have poor hygiene. There is also a lack of proper disposal of animal waste including inadequate drainage. Rural areas do not receive adequate health education. Some of the severe problems regarding health issues also arise from malnutrition around the country. There are only 35 out of 1000 live childbirths in the lower income strata of the country which is a major reason for the lack of nutrition among young mothers (Joarder, Chaudhury & Mannan, 2019, p.3). This is the direct cause of rapid population growth, inadequate food distribution, illiteracy, poverty and so on. Bangladesh also has a high-frequency tendency of flooding which leads to a huge amount of crop wastage every year.
Practising health in rural areas and countries like Bangladesh requires a clear understanding of the culture and customs of the society. The main reason behind it is most of the patients are not adequately educated and have notions and taboos about treatments. In such cases, the health practitioner must be patient and sensible towards the mindset of the patients, while also providing them with the right treatment (Adhikary et al., 2018, p.1). Moreover, the doctors and nurses also need to ensure that the patients come back for the treatment and do not get agitated by the health care providers.
.png)
Figure 3: Malnutrition in children in the last decade
Source: (Tradingeconomics, 2022, para. 2)
Conclusion
It can be concluded from this essay that Bangladesh is yet to cover a long path to reaching an ideal health care system. I have discussed my family's role and also the other families of the society who play a vital part in the healthcare system and it's uplifting. I have also compared my views with the data that I have collected regarding the health care system and the contribution of the government in various parts of the country. The role of the society has also been analysed to understand why Bangladesh is still behind in the healthcare scenario.
Reference List
.png)
.png)
NURS2193 Nursing Therapeutics and Aged Clients Assignment Sample
This assessment for assignment help requires you to use your academic writing skills to produce a 1500-word essay.
This will contribute to 50% of your overall mark for the course and supports several of the course learning outcomes for this course:
» CLO 2: Compare and contrast the various work contexts of the professional nurse
» CLO 3: Prepare written communication relative to the acquisition of nursing knowledge
» CLO 5: Describe the basic principles of reflective practice and evidence their application in relation to particular learning tasks
Essay Topics
Choose any 1 topic from 2.
1. Professional boundaries are an important feature of therapeutic relationships between nurses and patients. Discuss this statement. Within your essay, identify the difference between boundary violationsand boundary crossings and provide an example of each.
OR
2. Reflective practice is regarded as a key skill for nurses that enhance professional learning and growth. Discuss this statement Within your essay, comment on why reflective practice is valuable for nursing students and beginning registered nurses.
Solution
Nursing professionals need to engage with their patients or clients in a dynamic way that demands their participation in maintaining a healthy interaction with the patient ensuring the delivery of quality healthcare practice that is beneficial for the patient (Molina-Mula & Gallo-Estrada 2020). The behavior and relationship between the therapeutic nurses and the patient must be very consistent throughout the treatment and within a framework of professional boundaries. In this academic essay, a thorough discussion on the therapeutic nurse-patient relationship would be done followed by investigation of the importance of the professional boundaries and its importance in therapeutic care would be performed, the concepts of boundary crossing and boundary violation with several examples will be discussed throughout the next few paragraphs.
The therapeutic nurse and patient relationship are one of the foundation blocks in nursing care. Throughout the treatment period, the nurses need to maintain the trust, respect, privacy, and dignity of their patients (Hartley et al., 2020). The nurse-patient relationship is a goal-oriented and fruitful relationship that serves the best interests of the patient as well as for delivering quality care. The therapeutic nurse-patient relationship is based on several foundational pillars as follows- firstly, trust, the therapeutic nursing practitioners must build trust between dim and the patient to deliver the best possible care for them. Secondly, respect, the therapeutic nurse needs to have respect start the values and culture of the patient who they treat. Thirdly, intimacy; The physical, psychological as well as emotional intimacy is required to deliver therapeutic play care and which creates a barn ability in the nurse-patient relationship.
The therapeutic nurse-patient relationship is different from the personal relationship in many aspects such as this relationship is based on several regulations and codes of ethics as per the professional standards and it is entirely goal-oriented and different from the spontaneous or uncontrolled interest-seeking personal relationship (Slobogian, Giles & Rent, 2017).
Boundaries are an important parameter in the case of a therapeutic nurse-patient relationship and the nurses should provide the care while staying within the boundaries of the relationship. Proper knowledge, skills and guidance are extremely important in maintaining the professional relationship between the therapeutic nurses and their patients, which is quite different from the personal relationship, where there is no formal education, guidance or advanced preparation required (Kornhaber et al., 2016). Boundaries that are common in the professional sector will be discussed in the subsequent paragraph of this study.
The professional boundaries are the little window in between the therapeutic nurses inability to control power and indulgence and the patients situational vulnerability. The professional boundary in therapeutic nursing care ensures and determines the lines through which they are professional and therapeutic behaviors are guided and in rectifying any behavior whether intentional or unintentional that serves their own interest rather than the patients care need. The therapeutic nursing practitioners must maintain professional relationships and boundaries to be able to maintain play respectful consistent relationships with their patients throughout the length of their treatment phase. The duty of maintaining professional boundaries lies only with the nursing practitioners but not with the patient. The boundary has some major importance in the therapeutic relationships between healthcare professionals and patients.
The professional boundaries in the relationship between the therapeutic nurse and the patient exist because of ensuring the safety and better care for the patients. The nurses need to follow these boundaries in order to sharpen the best interest of the patient throughout their treatment period, it is beyond their personal characteristics and affection. During the therapeutic relationship with the patient, the therapeutic nurse has access to patient information and they can influence the patient seeking care. These specialized knowledge skills as well as access to personal data create a vulnerability for the nurses to the patient. To ensure that the code of ethics professional boundaries, as well as patient safety, are maintained the nursing practitioners must always remain within their professional boundaries during real life practice. In the subsequent paragraph of this study, the author will specifically focus on approaches that are followed to cross the professional boundary in therapeutic communication and relation.
Boundary crossing in a professional relationship between the therapeutic nurse and the patient could be explained by short misconduct as per the professional behavioral standards during their service for the therapeutic care of the patient. The boundary-crossing incidents as moderate to low significance when it occurs for the first instance but overtime with frequent occurrence of boundary-crossing crossings this may lead to boundary violation and which has a serious impact on the professional code of conduct ( Kristoffersen, 2019).
Several actions that lead to boundary crossings when the therapeutic nurse encounters a vulnerable patient are as follows: Maintaining a personal relationship with the patient. Connecting with the patient through social media. Intentionally disclosing in front of the patient. Maintaining a behavior of gif taking from the patients. Providing favors to the patient outside of the job roles and responsibility. Providing special care for the patient beyond the job role ( Hazen et al., 2018). Providing therapeutic care for friends and family
Boundary violation is a serious concern in the case of the therapeutic relationship between the nurse and the patient. Boundary violations are a clear persistent breach of professional boundaries and underlying trust between the patient and nurse. When the nurse takes advantage of the professional relationship they have with their patients and fulfill their personal needs that is a clear indication of boundary violation. Boundary violations are not acceptable in the therapeutic nursing practice and it can impact the nurse’s career affecting licensing sanctions ( Manral, Pareek & Kaur, 2018). The underlying cause of the boundary violation could also be the lack of understanding and confusion present between the nerds and the patient’s relationship in case of what is the roll-up the nurse and play the therapeutic needs of the patient
Several examples of boundary violations are as follows: Engaging in a romantic or sexual relationship with the patient under treatment. Self-disclosure beyond a certain limit with the patient. Lending money or borrowing money from the patient who is receiving the treatment from the therapeutic nurse. Maintaining a culture of gift taking and giving and asking for a favor in return. Asking for benefit what the nurse by influencing the client’s will or power. Too much involvement with the patient that impacts their personal relationship. Using the patient as a medium for selling or promoting the nurse’s own business. Engagement of the patient in providing care to the nursing practitioner.
The violation of professional boundaries between the therapeutic nurse and their patient has a serious impact on the patient as well as the nurse and on the overall patient care that is given. The professional boundaries are in place to help protect the patient’s valuable information and the safety of their treatment. When the professional boundary is breached there is potential harm to the patient which is not always immediately noticed or recognized. Due to this boundary crossing and violation the negative consequences are faced by the patient ( Hook & Devereux, 2018 ). The altered expectations and behaviors if not sustained and managed can create mentally as well as physical trauma to the patient and interfere with their treatment. Crossing professional boundaries as well as violating the boundaries has a serious impact on the nursing practitioner’s professional career. Lawful action may be taken against the nerds and termination of their employment could be enacted. The violation of professional boundaries also has serious physical and mental struggles for the nursing practitioners which lead to their lack of effort in the daily practice impaired personal relationship and stress ( Reyes Nieva, Ruan & Schiff, 2020 ).
This academic essay summarizes the relationship between the therapeutic nurse and their patients and several parameters associated with this. Boundary crossing and boundary violation with respect to the therapeutic nurse-patient relationship is defined followed by several examples which indicate the behaviors associated with boundary crossings and violation. The impact of boundary crossing and the violation has a play on patient care and patient safety as well as on the professional as well as the personal life of the therapeutic nursing practitioner is critically discussed in this essay.
References
.png)
PBHL20001 Understanding Public Health Assignment Sample
This assessment task for this unit is a reflective practice assignment of about 2000 words that describes your growing understanding of Public Health as a discipline. This is an individual assignment. You are strongly encouraged to work on your reflection throughout the term and to make notes of ideas that occur to you or issues that interest you that you can include when you write your assignment.
Your reflection should focus on how your understanding of Public Health changed over the course of the term, and you should compare your knowledge, perceptions, and attitudes at the beginning of this unit with how you feel at the end. You should also reflect specifically on the following questions:
1. How does an understanding of the history of Public Health contribute to professional practice?
2. How important are the non-health factors that are part of public health practice?
3. What are some of the ethical issues associated with public health practice?
4. How will the things you have learned as part of this unit affect your own practice in the future?
This reflective assignment is an essay. A less formal writing style may be used, and references are not required. If you do use any source material, however, each item must be identified in an in-text reference and also appear fully cited on a reference list.
Solution
Introduction
The concept of public health is very important as it deals with ensuring the health and wellbeing of all the people of a country. However, there are different aspects related to the public health related policies. These aspects may not be medical in nature. Factors such as social aspects and ethical issues can affect public health related decision making. In this context, this essay for assignment help will highlight the history of public health and its contribution to professional practices. Along with this, it will also highlight the ways in which social factors and ethical factors impact public health related decision making. Lastly, this essay will highlight the concepts that I have learned in relation to public health during my coursework.
1. An understanding of the history of Public Health and contribute to professional practice
History of public health had become important in the second half of the nineteenth century in the USA. By the late 19th century, in the USA a public healthcare structure had been established which helped me and healthcare staff to treat the patients with proper guidelines.
History of anything is important to understand the present value of the particular area. In healthcare, the history of public health plays an important role in understanding different aspects for professional practice (Naeem et al., 2021). Public healthcare is always involved with different kinds of risks. Due to different symptoms and different health conditions, there are risks of wrong treatments. Historical facts and information help to avoid such risks. Apart from that, history always shows the ways that have already been considered for public health. The result may be favourable or adverse for the patient. Thus, in order to provide better treatment to the public, healthcare organisations can bring up innovative ways to treat people. Innovation helps public healthcare to be more developed and advanced. With the advancement of Medical Science, public healthcare should also become more developed for the better health of the society.
For a doctor, it is important to know the history of healthcare. A person may have a family history of carrying a disease hereditary and that affects that person at a point of his or her life. In such cases, I should know about the family medical history to go forward with the most suitable treatment method. It helps me to consider the wider range of possibilities rather than narrowing the possible ways of the treatment (Aruru et al., 2021). The history of public healthcare helps me understand the timescale of beneficial health. Exceptions are there too as some of the communicable diseases do not follow the rules of history. Nevertheless, in order to improve the public healthcare activities, I should consider all kinds of facts and figures from the past to understand the nature of the disease more conveniently. It will help me to find relevance with the future plans too.
It is important for the healthcare units to keep a track of every vase of public healthcare to use it as a history of case studies in case of treating the same disease in future. For me, knowing the health history of the family of the patient can be fruitful as it helps me to take necessary steps in order to minimise the health risks of the patient (Estabrooks et al., 2018). For example, a family has a history of diabetes. It is being observed that the family members who are blood related, have a high chance of diabetes at a certain age. In this case, I always advise to have regular checkups and blood tests.
2. Importance of the non-health factors that are part of public health practice
Before enrolling for this course, I had an idea that the non-medical factors had no relation with public health practices. I was unaware of the different aspects of non-health factors and how these aspects can make or break the mere foundation of public healthcare. However, during this coursework I was introduced to this topic in depth. I have been taught that different social aspects such as level of income, level of social protection, food insecurity, education, unemployment, discrimination and social exclusion and others play an important role in public health care facilities (Ford and Airhihenbuwa, 2018). As per World Health Organisation, social determinants are more important than lifestyle choices when it comes to influencing health. We have read those undeveloped countries where the rate of uneducated people is higher face more public health issues. For example, the covid-19 pandemic has also affected the deprived section of the countries in larger proportion. There is a higher chance that people with low-income groups will not be able to get the same healthcare facilities that other people get. Moreover, there is a high chance that diagnosis of dieseases will be late for these people as they often avoid going for checkups (Schuchat et al., 2020). On the other hand, people with a low rate of education are not aware of the different healthcare initiatives. Moreover, they may not be aware of the precautions that they need to take. Factors like low income, higher rate of unemployment and lack of economic growth also leads to depression which can again lead to substance abuse and drinking. Lack of education and social awareness can also lead to taboos and stigmas which can make it difficult for the people to get access to healthcare.
During our coursework, we have also learnt about the different strategies that are being taken to mitigate these issues. I have noticed that governments of different countries have started to make health considerations while making decisions about all the other aspects of society. I think this policy is highly effective as it engages a diversified range of stakeholders and aligns their objectives of promoting health as well as social welfare (Khoury et al., 2018). During the coursework, I have been taught that focusing on job creation, development of agriculture, improving the educational system and ensuring equality can ultimately improve public health. In this context, I have noticed the government making policies for ensuring that there is full attendance in the schools while also ensuring that the students are being educated about different diseases and the way they can take care of themselves. This is a form of responsible learning. Moreover, I have learnt that implementing cross-sector strategies can also improve the health of neighbourhoods which belong to poor sections of the society (Brownson et al., 2018). I know about different coordinated strategies that have been implemented across different sectors with social, cultural, economic barriers. These sections of the society have health disparities and are making cross sectional policies to mitigate the same.
3. Some of the ethical issues associated with public health practice
Ethics is a branch of philosophy which differentiates between right and wrong actions. During my coursework, I have learnt about the ethical issues that can hamper public healthcare practices. As per my understanding, the different ethical concerns that arise in healthcare practices include informed consent, confidentiality, scientific integrity and respect for human rights. In this context, the public health ethics inquiry has three main functions, which include identifying and mitigating ethical dilemmas, resolving the dilemmas by deciding the most suitable course of actions (Wickramage et al., 2018). I have also learnt about different forms of ethics such as bioethics which deals with reproductive or end of life decision making, clinical research ethics, confidentiality and use of emerging technologies. Here, as a healthcare practitioner the focus needs to be given on whether the decision taken will be beneficiary for the patient or it will be non-malefic. Other than this, the concept of justice also plays an important role. This is the reason why female foeticide is banned in India. Moreover, gender determination is also banned in India due to the ethical grounds of healthcare. Moreover, I have knowledge that health care practitioners have the liability to safeguard patient information. Other than this, I have also learned about public health ethics which deals with emergency preparedness, social determinants of health, infectious disease control and others.
As per my knowledge, the covid-19 pandemic was a type of ethical issue for the public healthcare system of different countries as it was the duty of the government to collaborate with the health care practitioners in order to reduce the spread of this infectious disease. I think that setting priorities is highly important as the government as well as the public health practitioners need to identify the way they will allocate financial resources (Estabrooks et al., 2018). The policy makers need to negotiate between different ethical issues as they choose their competing priorities in order to resolve the conflict. Our coursework has also taught us about the five conditions that are developed by James Childress that have to be considered before overriding important morale considerations in healthcare. These are policy effectiveness, least restrictive infringements, proportionality of benefits and burdens, necessity and public justification. Thus, as far as I have understood, public health care has to be followed in alignment with asset goals, benefits and burdens of public healthcare and the actions associated with them.
I also think that the majority of public health practitioners do not have adequate skill sets to consider ethics in their day to day work. In this case, first the healthcare practitioners will have to let go of the normative assumptions they hold. Majority of healthcare practitioners think that relying on professional experience and own personal morale is more than enough in managing challenging ethical issues in healthcare (Khoury et al., 2018). However, in reality there is lack of proper clarification and the boundaries of ethical healthcare are also not properly set. The existing healthcare frameworks also do not have the ability to reduce ethical tensions. The decision makers need to formulate frameworks that can manage ethical conflicts while reducing ethical tensions. Thus, I have learnt from my coursework as well as personal experience that there is a lack of effective policies to mitigate the ethical challenges associated with public health. However, the government is trying to take active measures to mitigate the same on a real time basis.
4. Learned factors as part of this unit affect your own practice in the future
The history of public health plays a vital role in comprehending various facets of my professional practice in healthcare. Various types of dangers are constantly present in public healthcare. There is a danger of incorrect therapy due to a variety of symptoms and health issues. Facts and information from the past can help you avoid such dangers. Aside from that, history always demonstrates the approaches to public health that have already been examined (Brownson et al., 2018). The patient's outcome may be positive or negative. As a result, healthcare organisations can come up with novel ways to treat patients in order to give quality treatment to the general public. Innovation aids the development and advancement of public healthcare. As medical science advances, public healthcare should improve as well, for the betterment of the people's health.
We've also learned about the many ways being used to address these concerns as part of our study. I've noticed that governments in several countries have begun to consider health issues while making decisions concerning other elements of society. This policy, in my opinion, is very effective since it involves a wide range of stakeholders and aligns their goals of enhancing health and social welfare. Throughout my training, I was taught that focusing on job creation; agricultural growth, educational reform, and guaranteeing equality can all help to enhance public health.
In this context, I've noticed the government enacting laws to ensure full attendance in schools, as well as to ensure that pupils are educated about various ailments and how they may take care of themselves. This is an example of responsible education. Furthermore, I've discovered that employing cross-sector techniques can help improve the health of neighbourhoods in low-income areas (Brownson et al., 2018). I'm familiar with a variety of coordinated solutions that have been applied across several industries to overcome social, cultural, and economic constraints. Health disparities exist in these areas of society, and cross-sectional policies are being implemented to address them.
Ethics is a philosophical branch that distinguishes between right and wrong conduct. I learned about the ethical difficulties that can stymie public healthcare efforts during my education. Informed permission, confidentiality, scientific integrity, and respect for human rights are among the various ethical considerations that occur in healthcare procedures, according to my understanding (Naeem et al., 2021). In this setting, the public health ethics inquiry serves three key purposes: detecting and minimising ethical issues, and resolving the dilemmas by determining the best course of action.
As a healthcare provider, my focus should be on whether the decision you make will be beneficial to the patient or non-beneficial. Aside from that, the concept of justice plays a significant role. Female foeticide is illegal in India for this reason (Wickramage et al., 2018). Gender determination is likewise prohibited in India because to ethical considerations in healthcare. Furthermore, I am aware that health-care professionals are responsible for protecting patient information. Aside from that, I have learnt about public health ethics, which includes topics like emergency preparedness, socioeconomic determinants of health, and infectious disease control.
Conclusion
After analysis, it has been concluded that heath care sectors need to inform their employees about different issues and make an awareness program. If the sectors want to improve its issues then it needs to make more charity programs and develop clinical leadership. Through those analyses understand various things and try to practice those days by day to improve it. I need to make my decision-making process more effective for the patient's benefit. I also think that fundamentals growth and education growth can help to develop heaths care services. Non-heaths factors did not have any concern with the heaths care sectors or services.
Reference list
.png)
NURBN1015 Introduction to Evidence-based Practice and Research Assignment Sample
Assignment Brief
This assessment task requires you to build on the evidence you summarised and evaluated in Assessment task 2a in order to respond to the clinical question in the form of an essay. The clinical question you chose for task 2a must be used for assessment task 2b. You will need to use at least SIX (6) peer-reviewed primary research articles in total. THREE (3) of these articles will be the three you used in the annotated bibliography, and you need to source at least THREE MORE articles yourself.
CLINICAL SCENARIO CHOICE – USE THE SAME CHOICE AS TASK 2A
Choose the same topic you used to complete Assessment tasks 2a.
Clinical scenario choice 1: Pressure injury prevention
Dario is a student nurse working in an aged care facility and is looking after Mr George Florentine an 82-year old man who suffered a stroke four months ago. He is not able to mobilise without assistance. It was handed over that Mr Florentine needs re-positioning every 2 hours. However, Dario’s buddy nurse says that is not necessary as he has a pressure relieving mattress.
Clinical scenario choice 2: Nutrition in wound healing
Amelia is a student nurse working in a residential facility caring for Iris Johnson a 92-year-old female with a ulcerative wound to her left lateral malleolus. The ulcer is 2cm in diameter and sloughy in appearance with minimal hemoserous exudate. Iris has been prescribed vitamin D and folic acid supplements to help with the healing process; however Amelia’s buddy nurse says that this is silly because nutrition has nothing to do with wound healing.
WORD LIMIT
The word limit is 1500 words (+/- 10%). The reference list is not included in the word count. In-text citations are included in the word count.
ESSAY STRUCTURE
The ‘applying evidence to practice’ essay is to be written using an essay structure with an introduction, a body, and a conclusion. The essay format provides you the opportunity to concisely present the findings from the research articles that directly respond to the clinical question/s, compare and contrast the findings, and then apply what is known to your own clinical nursing practice.
The essay should be structured as follows - do not include headings/subheadings in your submission:
Write the clinical question you have developed from the chosen scenario at the top of your essay – this is your essay title.
Introduction: Word limit allocation (approximately) 150 words
What to include
Introduce the topic (the clinical question you are answering), outline the scope of the paper (what you will cover) e.g., evidence-based strategies, how they are applied and evaluated (follow the paragraph topics below)
Paragraph 1: Word limit allocation (approximately) 300 words
What to include
What new knowledge from the research studies can be applied to improve nursing care or patient outcomes?
Compare and contrast findings – paragraph 1.
Paragraph 2: Word limit allocation (approximately) 300 words
What to include
Compare and contrast findings – paragraph 2.
Paragraph 3: Word limit allocation (approximately) 300 words
What to include
Apply this new knowledge from paragraphs 1 and 2 to nursing practice: What strategies will you use to implement new knowledge into patient care?
Paragraph 4: Word limit allocation (approximately) 300 words
What to include
State the methods you can use to demonstrate that nursing practice or patient care is improved.
Conclusion: Word limit allocation (approximately) 150 words
What to include
Summary of the main points
Reference list: (Not included in word count)
Include all references used in text in APA 7th style
Total word count = 1500 (+/-10%)
ESSAY PREENTATION GUIDELINES
Solution
Brief introduction
Immobility, such as that brought on by protracted bed rest at a medical facility, can lead to pressure injuries also termed as bedsores. Most pressure injuries are preventable, and they contribute significantly to patient treatment needs in the healthcare industry. Pressure damage is included on the national list of hospital acquired problems (HACs). The national list of 16 HACs is the product of a detailed methodology that involves literature reviews, clinical interaction, and concept testing with both public and private institutions (Hajhosseini et al., 2020). The hips, heels, tailbone, elbows, head, and ankles are among the skeletal parts of the body that are commonly the locations of these injuries. Pressure injuries can be treated in a number of ways, depending on the stage. Once the wound's stage and severity have been determined, it must be cleaned, frequently with a saline solution (Dalvand et al., 2018). After being cleaned, the wound has to be kept clean, moist, and properly wrapped. To cover the wound, the doctor may select from a range of bandages. This assignment would help to understand the preventive measures that must be taken to prevent the chances of pressure injury.
Body paragraph 1
Topic sentence: Keeping the skin clean and clear of bodily fluids can prevent pressure injury
Evidence: The first stage in skin care is routine assessment of the skin itself. In high-friction areas, patients and/or caregivers should pay careful attention to the skin and keep it dry, clean, and protected from pressure injuries by keeping an eye out for early warning signs (especially at high-pressure spots). Sensors can alert patients or caregivers to any changes in the environment that can make pressure injuries more likely to occur (Jiang et al., 2020). These sophisticated monitoring techniques include pressure mapping and real-time patient monitoring. This is an opportunity for early management and the reduction of pressure injuries for assignment help.
The following best practices for skin care in this patient population are recommended are every day, examining the skin, moisturizing at least twice daily to keep the lipid barriers functioning optimally, using additional skin barriers if the patient experiences incontinence, cleansing, rinsing, and drying the skin after incontinence or when there is too much moisture present, to cushion and protect sensitive areas, using the appropriate therapies, and whenever necessary, or every two hours, changing into breathable clothes (Cox et al., 2018). Dressings are one pressure ulcer therapy strategy. There are many different types of dressings, and they can range widely in price (Sala et al., 2021). Hydrogel dressing is one type of available dressing. The high-water content of hydrogel dressings keeps ulcers moist, preventing them from drying out. According to popular belief, wet wounds heal more quickly than dry ones. Numerous research has examined the possibility that hydrogel dressings for pressure ulcers have a faster rate of healing than other kinds of dressings or topical treatments (Alderden et al., 2018).
Body paragraph 2
Topic sentence: Pressure Redistribution resulting in pressure relief might help to prevent pressure injury
Evidence: Pressure injuries can be avoided by controlling friction and shear. There are mainly two approaches to doing this. The first step entails choosing the optimum materials for the patient's surroundings and support surfaces like beds, mattresses, and cushions. Equal weight redistribution is another goal of these support surfaces. The choice of fabric can also significantly affect how much mechanical stress the patient receives; for instance, it has been demonstrated that textiles made of silk have far lower friction forces than fabrics made of cotton (Padula et al., 2019). On pressure redistribution surfaces, skin contact is increased, resulting in a continuous, even IP. The best material for foam and low-air-loss mattresses is this one. Polyurethane foams that are lightweight are made to contour to the patient's body and account for pressure points in certain areas. With pressure redistribution incorporated directly into their characteristic shapes, cut-foam mattresses and laminated surfaces are only two examples of the increasingly sophisticated material architectures that have resulted from this. Low pressure treatment mattresses also offer pressure redistribution since they continually circulate low air pressure throughout the mattress to spread the user's weight. It is comparable to low air loss therapy, with the exception that the air is kept in the mattress to prevent full deflation when the pump is switched off (Cox et al., 2020). Pressure relief effectively prevents pressure accumulations by focusing on high pressure areas of the body. These surfaces typically contain air-filled cells that might expand and contract based on the surrounding conditions (Fulbrook et al., 2019). For instance, it may be useful to regularly reduce pressure in the lowest third of the mattress if the patient's heels and lower legs are more prone to pressure sores when lying on a mattress. In this case, alternate-air technology can be useful. This cyclical mechanism uniformly distributes pressure over the mattress in response to the patient's needs, reducing the chance of pressure buildups for a lengthy period of time (which also gives the mattress an undulating IP measurement).
Body paragraph 3
Topic sentence: Repositioning of the patient would help to reduce pressure injury
Evidence: Another element of effectively managing mechanical stress is repositioning the patient as needed, ideally every two hours (Sharp et al., 2019). To alert the patient or the staff when repositioning is necessary, auditory aids like alarms or sensors may be used. Repositioning may also be assisted by tools, pillows, or slings that make it easier to move the patient. The application of pressure mapping technologies can also help with patient positioning. This device enhances the visual assessment of a patient's skin by examining the cellular-level processes and biomarkers connected to the early formation of pressure ulcers (De Meyer et al., 2019). Patient positioning includes maintaining neutral body alignment in compliance with the requirements of the treatment. It is accomplished by preventing hyperextension and excessive lateral rotation. Because it lowers the possibility of harm and the negative effects of immobility, proper patient placement is an essential aspect of nursing. Correct patient positioning optimizes exposure to the treatment region while minimizing exposure. Furthermore, there is no evidence that gradually shifting one's position or weight would affect how much pressure is applied at the contact between the sacrum and buttocks (Yap et al., 2022). However, there is evidence that even little adjustments to weight or posture can have an impact on the gravitational equilibrium. Further research must be done to determine how well modest modifications to weight or posture might minimize pressure injuries in patients receiving critical care.
Body paragraph 4
Topic sentence: Usage of medical devices and physical barriers can prevent pressure injury
Evidence: Any object that comes into contact with the patient's skin might result in a pressure injury. This is compounded worse in the pediatric inpatient environment where device-related pressure injuries account for the majority of all pediatric pressure injuries due to the underdeveloped skin barrier and decreased tissue tolerance (Lin et al., 2020). As medical care becomes more complex and includes more devices, nurses must effectively assess patients' requirements and protect patients' skin from getting device-related pressure injuries. creating a physical barrier that shields moisture and irritants from the skin's health and regeneration. By producing a transparent barrier, the wipes lessen diaper rash and skin irritation caused by incontinence without altering the absorbency of incontinence products (Padula et al., 2021). Barrier wipes have been shown to minimize redness and discomfort when used in diaper cares by avoiding breakdown and may be applied similarly to traditional barrier lotions. Barrier wipes do not need to be removed and permit ongoing integumentary examinations.
In addition to the aforementioned fundamental measures, patients and caregivers should pay particular attention to food and water. People who are undernourished are far more susceptible to get pressure injuries. A healthy diet that is balanced, enough hydration, and the use of supplements as needed can all significantly reduce the incidence of pressure injuries in patients (Munoz et al., 2020).
Brief conclusion
From the above discussion it can be concluded that pressure injuries occur when pressure causes a localized damage to the underlying skin and soft tissue. Hospitals and long-term care facilities continue to have a lot of concerns about these skin and soft tissue injuries. They are costly for patients and in the healthcare system, and they have a detrimental effect on patients' quality of life. If the considerable morbidity and death rates linked to these pressure injuries are to be avoided, they must be immediately identified and treated. When different kinds of tension are applied to the skin's surface, a pressure injury happens. When dealing with a pressure injury, infection prevention is essential. If the wound becomes infected, the rest of the body might be in risk. Pressure injuries should be avoided whenever practical since they could have a negative effect on patient outcomes. The first measures in preventing pressure injuries are a comprehensive skin assessment and suitable skin care. Making a management decision for pressure injuries will be aided by the assessment of patients upon arrival. Care plans may also include other things like moisturizing the skin, protecting bony prominences, shielding it from dampness, redistributing pressure, and more.
References
NUR5011 Contemporary Nursing Assignment Sample
Mr George is a 65 year old widowed father of Giovanni and Maria. He was admitted to your ward for elective lumbar surgery after several years of back pain resulting from a workplace injury. His ability to mobilise has been significantly reduced and he uses a walking aid. Mr George does not speak English and relies on his son to translate for him.
Mr Georges admission paperwork was completed with Giovanni’s assistance. Mr George is allergic to morphine. Giovanni thinks it caused an itchy rash, but Mr George cannot recall. RN Sriya has written this in the paperwork but forgot to put on a red allergy wrist band. His neurological limb assessment shows a left foot drop with full feet numbness and his vital signs are unremarkable. Mr George has a past history of atrial fibrillation. He is on digoxin (0.25 mg/day) and aspirin (100 mg/day). He is noted to be on the organ donor register and Giovanni is the documented medical treatment decision maker.
Giovanni has advised that his father does not wish to be resuscitated in an emergency, but Giovanni is not supportive of this and would like all measures taken. Giovanni has also advised that Mr George is quite anxious about his brother, Steven who is also in the hospital, having been admitted for surgery after falling in the garden. Professor Charcot, the surgeon, visited Mr George and Giovanni on the ward to see that Mr George is settling in well and reminded Mr George and Giovanni that he would perform an L2/3 laminectomy the following morning. RN Kate looked after Mr George on night shift but had difficulty communicating with him. As she thought he might have had a stroke, she placed an electronic order for an emergency CT Brain. In her hand over to the AM nurse (RN Chan), she advised that the CT results were not back but did not documented this.
When RN Chan took Mr George to theatre, they noted that a consent form signed by the patient and the surgeon was not in the file and inserted a blank form into the file for completion. RN Chan alerted Professor Charcot to this. Professor Charcot responded by yelling at RN Chan in front of other nurses and surgeons “You’re so incompetent. Who do you think you are?
If you dare speak to me like that again I will have you fired! Of course, I have already consented the patient! He would not be here if he did not know what was happening. Are you the idiot who ordered a CT Brain on my patient?. RN Chan returned to the ward, upset. They told their manager what had occurred and that they felt bullied and harassed by Professor Charcot. After surgery when Mr George returned to the ward, RN Chan noticed that the hospital consent form had still not been signed and when listening to the Registrars talking to each other about the case, overheard one say, Prof didn’t use xray and did the L4/5 by mistake. RN Chan did not say anything to their manager as they thought that the doctors would advise the patient and his son. They were also too scared to say anything because they didn’t want to be yelled at further and lose their job.
RN Chan went home very upset at the day’s events and wrote on their Facebook status update that “some surgeons are so arrogant! At least I am not the incompetent surgeon who operated on the wrong spinal level!” During the next shift and about 8 hours after surgery, it was noted by the PM nurse, RN Sriya, that Mr George had not passed urine. The protocol of the hospital requires a urinary catheter be inserted if the patient has not passed urine 8 hours after spinal surgery. RN Sriya contacted the Registrar who advised she could not arrive to insert the catheter for 2 hours as she was in surgery with another surgeon and that RN Sriya would have to do it herself. RN Sriya had not inserted a catheter into a male patient before and, assuming it couldn’t be much different to inserting female catheters, undertook the procedure. As a result, frank haematuria occurred with a large amount of blood loss. A MET (Medical Emergency Team) was called, and the patient assessed. Mr George was in a lot of pain and the attending MET doctor, Dr. Pratt orders 5mg of morphine intravenously stat. Mr George was rushed to emergency theatre and a Urologist, Miss O’Donnell, called to surgically repair the damaged urethra. During the operation Mr George went into cardiac arrest and died.
When Giovanni and Maria arrived at the hospital to see their father, RN Sriya asked “Didn’t they call you? He died in the operation”. Maria was understandably angry and upset and stated “No one called me! I am going to sue the hospital and Professor Charcot for negligence, and I am going to the coroner, media, and escalating this as far as I can take it!”.
The case study is designed to prompt your thinking and analysis of the various legal issues/considerations that may arise in health care. Please note that you are not asked to provide a personal view of the case study. The purpose of the essay is to present a coherent argument for the legal considerations that are relevant to the case study. This essay provides an opportunity for you to demonstrate in-depth understanding, and sound, logical and academic argument to support your thoughtful position on the legal considerations present in the scenario.
Structure: Your essay should follow the parameters of the marking rubric; You may use subheadings to develop your paper; The suggested assessment structure in line
- Introduction: should clearly introduce the assessment task and provide an outline of your essay
- Main body: the argument for each of the legal considerations is developed logically & demonstrates critical analysis. It is recommended that the body of your essay is separated into the three legal issues.
Conclusion: summarises the main points of your essay.
Solution
Introduction
In Australia, both the government and the private sector provide healthcare. The Nursing and Midwifery Board of Australia (NMBA) registration is mandatory for nurses seeking employment in Australia. Every Australian nurse must adhere to the NMBA's code of conduct. This article outlines the professional and ethical requirements for Australian nurses. The nursing profession is controlled by both customary and legislative laws. These laws include the Nurses Act, the Health Practitioner Regulation National Law, and the Privacy Act, among others (Harrison, 2018). Common law is the body of law that develops through judicial decisions. Professor Charcot often disregarded the responsibility of care he owed to Mr. George. He failed to get Mr. George's consent for the therapy, performed surgery on the improper level of the spine, and threatened and mistreated RN Sriya throughout the procedure. During each of these complications, the patient was anaesthetized.
The hospital's incapacity to provide its patients with adequate care may also be asserted. The hospital did not take sufficient measures to verify that the required authorization form was filled out and that Sriya, the RN, had enough training in the implantation of urinary catheters. Furthermore, no effort was taken to inform Mr. George of the potential risks associated with the treatment. The complaint must establish that the alleged loss or damage was directly caused by the alleged breach of duty (Dixit & Sambasivan, 2018).
Legal Issue 1: Negligence
Specialists, such as surgeons, may often commit the tort of negligence on the job. The term "tort" is often used to refer to reckless behaviour. It happens when a professional breaches their duty of care and causes damage to a patient. The patient alleges professional negligence has the burden of proving that the professional owed them a duty of care, that the obligation was breached, and that the loss or harm was caused by the breach.
A professional has a reasonable duty of care to the patient under their care, which requires them to take all reasonable precautions to avoid harming the patient. Regarding surgery, this entails taking all necessary steps to guarantee that the right patient receives the correct therapy and that the patient is aware of any potential dangers (Buss et al., 2018).
In this scenario, Professor Charcot's actions might be seen as a breach of his duty of care owed to Mr. George. The first problem was that he was unable to convince Mr. George to agree to the therapy. The second error was operating on the wrong portion of the patient's spine. Thirdly, he failed to inform RN Sriya about Mr. George's possibly fatal allergy to morphine. Fourth, he persistently harassed and intimidated RN Chan.
In addition, due to Mr. George, the hospital may have violated its duty of care on many occasions. It did not thoroughly verify that a legitimate authorization form was submitted and signed. The second worry is that RN Sriya was not adequately screened to ensure she has the required skills to insert urinary catheters (Rosebrock et al., 2020). Thirdly, nothing was done to ensure that Mr. George was informed of the dangers involved with the procedure, which would have been considered reasonable under the circumstances. The complaint must establish that the alleged loss or damage was directly caused by the alleged breach of duty. In this case, the loss or damage at issue is Mr. George's death. If Professor Charcot hadn't been so careless, Mr. George would be alive and well today. If he had gotten adequate care and been informed of the risks, he could have lived. If the hospital had been more responsible, Mr. George may still be alive today. Mr. George would have gotten proper care, a valid permission form would have been completed, and he would have been informed of the possible hazards of the surgery if the hospital had been more diligent.
The Health and Safety at Work Act of 1974 (HSWA 1974) mandates that companies preserve the health and safety of their employees at work. This obligation for assignment help involves protecting workers from intimidation and harassment (Chun Tie et al., 2018). It is hard to establish whether the hospital exceeded its obligation by failing to take adequate safeguards to protect RN Sriya from intimidation and harassment by Professor Charcot. Alternatively, it is likely that the hospital ignored this requirement.Under the Health and Safety at Work etc. Act of 1974, employers are required to ensure the health, safety, and welfare of their employees in the workplace to the greatest degree practical (HSWA, 1974). This duty comprises safeguarding employees against intimidation and harassment in the workplace. It is arguable whether the hospital breached its duty by failing to take enough safeguards to protect RN Sriya from intimidation and harassment by Professor Charcot. It is possible, however, that medical workers neglected their responsibility.
Professionals, such as surgeons, may incur the tort of negligence in the course of their employment. Liability results from a violation of the professional's duty of care to the patient, which results in the patient suffering some kind of harm. Patients who allege medical professionals broke a duty of care due to them must also demonstrate that the violation directly resulted in the losses or damages they're seeking compensation for.
A professional owes their patient a duty of reasonable care, which entails doing all in their power to prevent the patient from suffering any damage that may reasonably be expected to result from the professional's actions. For a surgeon, this means taking all necessary precautions before surgery, such as checking the patient's identity and medical history to make sure they are a good candidate for the treatment and explaining the potential dangers to the patient.
The most common tort faced by healthcare personnel is carelessness. The patient may suffer physical hurt, pathological harm, mental harm, or even death as a consequence of the nurse's carelessness. Damages are incurred when something terrible happens, such as an accident induced by medical treatment that prolongs a patient's hospital stay and/or leaves them permanently incapacitated after discharge, or even causes death. This sequence of events begins with the imposition of a duty of care and continues through the exercise of inadequate or non-existent care (henceforth termed "negligence"), the occurrence of an adverse event, and the inflicting of injury. In cases of negligence or wrongdoing, the court may award damages to the injured party. In some circumstances, a negligent person may be held accountable for compensating damages to compensate for economic or non-economic losses, in addition to extraordinary damages. Long ago, carelessness was characterized by common law. In 2002, in response to the conclusions of Justice Ipp, all Australian jurisdictions enacted Civil Liability Acts with provisions addressing medico-legal malpractice (Cross& Cross, 2020).
Employers have a responsibility to protect their workers' health, safety, and welfare as much as possible under the Health and Safety at Work Act of 1974 (HSWA). This obligation includes safeguarding workers from hostile work environments. It might be argued that the hospital in this instance failed in its obligation to safeguard RN Sriya from the bullying and harassment of Professor Charcot.
The obligation to guarantee, so far as is practically feasible, the health, safety, and welfare of workers at work is imposed on employers by the Health and Safety at Work etc. Act 1974 (HSWA 1974). This obligation includes taking measures to prevent bullying and harassment of staff members. It might be argued that the hospital in this instance failed in its obligation to provide RN Sriya with enough protection from the bullying and harassment of Professor Charcot.
Patients like Mr. George who have been injured by unintended side effects may or may not choose to file a lawsuit. Patients who successfully obtained compensation may not have been under the supervision of a nurse at the time of the occurrence. Unbelievably frequent prescription errors and failures to recognize negative consequences among Australian healthcare practitioners are among the most serious concerns affecting the nation's patients. There is a surprising mismatch between the reported occurrence of medical misbehaviour and the amount of money paid out in settlements, according to new statistics on negligence claims in Australia. according to current research, the number of new claims submitted has decreased, or the pace of new claims has remained constant (Kirkegaard et al., 2022). The effectiveness of conflict resolution is growing. There is tension between the need to maintain a high standard of care and the prevalent practice of rewarding patients for unexpected outcomes. In contrast to their colleagues in New Zealand, who have access to a no-fault medical reparations scheme, health professionals in Australia must adhere to common law and statute-based negligence regimes.
As a basis for responsibility, carelessness is rapidly extending to all spheres of human activity and is today the most important and pervasive tort. In recent decades, the legal notion of carelessness has expanded to include economic loss and psychological illnesses in addition to bodily suffering and property damage. In order to achieve justice and lessen the burden on society as a whole, it was difficult but necessary to develop a legal system that is both predictable and consistent.
Despite the fact that each doctor has a unique set of beliefs and values, they are all bound by a set of professional standards that serve as the foundation of their work. Doctors must always act in the best interests of their patients and adhere to the most stringent standards of safe and effective care. They must be dependable and possess a solid moral compass. Patients have faith in their doctors because they perceive them to possess not just the required medical expertise, but also exemplary character traits such as honesty, dependability, and compassion. Patients have confidence in their doctors and expect them to safeguard their confidentiality. Physicians are obligated to safeguard and enhance their patients and the general public's health. In a successful medical facility, the patient’s needs are always first. Medical practitioners must recognize that each patient is unique and collaborate with patients to adjust therapy to each individual's requirements and goals. This requires cultural awareness, which includes knowing and respecting one's own culture and values as well as those of others, and recognizing that cultural differences may affect the doctor-patient interaction and the delivery of health care. Every aspect of safe and effective medical care requires superior communication (Sotomayor-Castillo et al., 2021).
Legal Issue 2: Misconduct
The "right to be treated with dignity and respect" refers to a patient's legal entitlement to treatment that respects and upholds their inherent worth as a person. Patients have the freedom to refuse medical practitioners' degrading or disrespectful treatment. This privilege was thus created for this purpose (Broom et al., 2022). Professor Charcot was the aggressor in the continuous bullying and harassment issue between RN Chan and Professor Charcot.
A physician is not required to provide care to anybody who seeks it, but he must be prepared to meet injured or unwell patients at any time. His duty is to offer compassionate treatment to his patients. Unless required by law, the confidentiality of a patient's medical records must always be maintained. Without exaggerating or trivializing, he must convey the gravity of the patient's illness. Once a patient has been admitted to the hospital, they must not be forgotten (Fisher et al., 2022).
When decisions concerning terminal care are made without comprehensive information or without engaging the patient or the patient's family, both ethics and the law are put to the test. Certain decisions regarding Mr. George seem to have been made without his complete consent or awareness. In addition, it seems that Mr. George and his family were not supplied with crucial information, which led them to believe they had been misled and lose faith in the medical professionals' abilities to care for them (Zheng et al., 2021).
Respecting the dying person's right to autonomy is crucial while making decisions concerning their care. Patients should participate in treatment decisions to the extent that they are able and willing to do so. Consent based on education is a crucial part of this operation, and it is essential that the patient has all the information necessary to make an educated decision. If the patient is incapable of making decisions, family members should be included.It seems that Mr. George was not given sufficient information to make an informed decision about the treatment he would receive. This is troublesome given the circumstances since it suggests that his autonomy was not respected (Minnican& O’Toole, 2020). In addition, it seems that Giovanni was not given all the information he need to make an informed decision on his father's treatment. In the case of an emergency, Giovanni would not have been able to make an informed decision on his father's resuscitation, which is problematic for a variety of reasons.
It is feasible for doctors, nurses, and other medical professionals to use their specialized knowledge outside of their regular work environment. Some physicians may not fully appreciate the responsibilities of medical professionals outside of their expertise. If there is no established therapeutic relationship between a doctor and patient and the doctor has no intention of aiding, one of three outcomes may occur (Gao, 2021). It is conceivable for a doctor to assert they are one but refuse to assist in any way, to acknowledge they are one but refuse to identify themselves as one, or to vehemently deny they are one. Regardless of ethical problems, a physician's actions and public image may have significant legal consequences. Elements of state legislation related to legal duties to aid, which vary widely from state to state, have been recommended for national study and revision.
The doctor-patient relationship can only endure if both parties adhere to the highest professional standards. This needs impeccable manners, respect for others, compassion, and honesty, all of which must be shown. Keeping in mind that every patient is unique Except for exceptional circumstances such as where disclosure is required by law or is in the public interest, respecting patients' right to privacy and keeping their medical information confidential. Patients and, if appropriate, their family members who help them manage their health care should be encouraged and supported in their attempts to become active participants in their own health care (Burström, 2022). Supporting and assisting patients in their efforts to improve their health literacy and make decisions based on enhanced information about their conditions and treatment options is essential in patient care. recognizing the power dynamic between doctor and patient and abstaining from exploiting the patient in any manner (including but not limited to physical, emotional, sexual, or financial means). When a doctor and patient are able to communicate successfully, their connection becomes stronger. This means not just listening to the patient, but also responding to their health-related worries and goals. You should inquire about your patients' use of conventional, alternative, and complementary therapy, as well as any other health recommendations. They should include any other health recommendations they have received. Patients should be given enough opportunity to contest or reject intervention and treatment, and they should be informed of the nature and need of all aspects of their clinical care, including exams and investigations. The process of teaching patients about their illness and available treatment options, including the advantages and disadvantages of each (Vardoulakis, 2021). Assuring that the patient has understood the information provided and is aware of any significant risks associated with any component of the treatment plan suggested for their illness. When possible, accommodate patients' special linguistic, cultural, and communication needs, and be aware of how these needs affect patients' ability to comprehend what is being communicated; respond to patients' questions and keep them abreast of the progression of their clinical condition. Learn about and use qualified language interpreters and cultural interpreters to meet the linguistic and cultural needs of your patients. The Department of Immigration and Citizenship provides a website providing information about government-funded translation services in Australia (Allen et al., 2020).
When all employees involved in a patient's care are able to communicate efficiently and treat one another with respect and compassion, the quality of care offered to the patient is enhanced. Transparent, efficient, amicable, and prompt communication with the other medical personnel and doctors caring for the patient is essential to the success of medical practice. recognizing and celebrating the efforts of everyone involved in a patient's care Maintaining a professional and courteous manner at all times, particularly while conversing online with coworkers. suggesting, allocating, and transferring work to others You may delegate care by requesting another healthcare practitioner to treat the patient in your place; but, you will retain ultimate responsibility for the patient's health (Kirkegaard et al., 2022). If a patient needs a second opinion or specialized care, their primary care physician may refer them to a specialist. When you refer a patient, you normally delegate (at least a portion of) the patient's care to another medical professional, either temporarily or permanently, depending on the circumstances, such as when the patient requires treatment outside of your area of expertise. The phrase "handover" refers to the transfer of full responsibility for patient care from one healthcare practitioner to another. A good medical practice consists of taking all steps to ensure that the individual you are entrusting with a task has the training, skills, and experience to provide the level of care you expect (Osborn et al., 2022). Remember that even if you absolve yourself of responsibility for the choices and actions of those to whom you delegate authority, you will still be held accountable for the overall care of the patient and your decision to distribute authority. This is true despite the fact that you will absolve yourself of accountability for the behaviour of people to whom you have delegated power. Never break the chain of continuous care for a patient by failing to provide pertinent information about the patient and the necessary treatment by failing to give the necessary information.
Legal Issue 3: Consent
In this instance, the nurses' actions have far-reaching ramifications that may be pursued via the judicial system. According to all parties concerned, Mr. George did not provide authorization for the procedure that was performed on him. Because his rights have been infringed, he may opt to file a lawsuit against the hospital and the physician. Consent based on education is a crucial part of this operation, and it is essential that the patient has all the information necessary to make an educated decision. Certain choices concerning Mr. George were made without his knowledge or consent (James et al., 2021). It had a bad influence on him as a result. This is troublesome given the circumstances since it suggests that his autonomy was not respected. Mr. George's experience highlights the need of making ethically and legally sound choices regarding end-of-life care. It is essential to respect patients' preferences and give them all the information they want to make an informed decision (Penman & Tighe, 2019).
As the situation presents, it is debatable whether or not Professor Charcot acted responsibly toward Mr. George. The first problem was that he didn't bother to get Mr. George's approval for the operation. Second, he cut into the patient's spine at the improper level. Third, he didn't do enough to make sure RN Sriya knew of Mr. George's morphine sensitivity. And last, he harassed and threatened RN Chan. The hospital may have broken its duty of care to Mr. George in various ways. To begin with, it didn't check to see whether the right permission form was signed. Second, it didn't check whether RN Sriya had had enough instruction on how to place urinary catheters. Third, it didn't do enough to warn Mr. George about potential complications from the operation. All of the plaintiff's suffering must have resulted from the defendant's alleged breach of duty. The death of Mr. George is the alleged loss or injury in this lawsuit. It might be argued that if Professor Charcot had followed protocol and warned Mr. George of the potential dangers, Mr. George would still be alive today. Mr. George may not have died if he had received the appropriate treatment, signed the appropriate permission form, and been informed of the potential consequences of his decision, all of which were overlooked due to the hospital's carelessness.
Consent is one of the mandatory requirements in a healthcare setting as it ensures the patient or the particular individual is aware of the actions that will be considered. It will help to avoid legal tribunals in case of any misery. From the following case study, it has been observed that Professor Charcot was too much arrogant and without any consent, he performs critical surgery to the patient Mr. George. After the action, the patient encountered severe physical issues due to the inability to urinate and died facing severe pain and medical complexity. It also indicates a lack of duty of care which is a major legal issue. As per the study of Yildirim et al, (2021), it is mandatory for any medical professionals to sign proper consent before proceeding with medical operations that might lead to serious consequences. The same is missing in the case which was found the very next day when RN Sriya was on duty for the next shift. Due to such actions, the family members and relatives claim that they will lodge complaints against all the staff. Despite informing by juniors about the consent the professor acts in his own interest. It is clearly a violation of National Human Right Committee guidelines. Therefore, as per this regulatory and legal framework also the medical practitioner is responsible for the punishable offences.
Considering the perception of the family members l, they are not wrong as none of them is informed about the consent or any of them are not aware of the serious condition or death of the patient. Here, the legal issue associated with lack of duty of care also comes into the picture. As opined by Waterhouse, (2019), the guidelines of "duty of care" clearly indicate that if any casualties occur due to any kind of negligence of individuals assigned in the responsibility, then the other party can sue. Hence, as per this rule, the hospital authorities might face serious legal consequences if the family members of Mr. George claim. However, the claim will be much stronger if it will be against the professor because from the case study it has been found that he is the main culprit.
Informed consent clearly indicates that both parties agree with the terms and conditions along with the consequences of the actions (Nouwens et al. 2020). In the following case, there is no question about the acceptance as no consent has been provided. Apart from that, there was also no verbal confirmation from the patient on the basis of which the entire result can be considered a consequence of the contract. Apart from that, as per the contract law, all medical professionals must check all patient-related documentation before considering any serious actions. In the current case scenario, it has been found that rather than checking the updated medical records the professor had considered the treatment actions that finally resulted in the death of the patient. Therefore, as per the contract law also the professor is guilty.
The case study reflects that there is a linguistic barrier associated with Mr. George as he was unable to understand English properly. As per the knowledge of Gerke et al., (2020), any linguistic challenge makes informed consent invalid as it does not serve the purpose of complete understanding. Hence, in that case, it was the responsibility of the medical professionals at the health care to elaborate everything to the patient. Then the criteria of verbal acceptance can be fulfilled which might lead to less legal trouble. Apart from that, it was also the responsibility of the medical professionals to discuss everything in front of the translator. Then it would make the understanding level superior that could be better to fulfil the criteria for informed consent.
From the case study it has been observed that l, there is no concern about the perception of Mr. George. Medical professionals execute their work as per their own interests. It is also a violation of consent guidelines. According to Döhlaet al. (2020), informed consent endures all the actions or experimentation that will be done, with the permission of the individual. As approval is missing in the case, therefore, it can be also counted as a legal issue associated with the context of consent.
The case study indicates that the professor threatened RN Chan with interference. It was her duty to inform the professor as well as it also falls under the basic rights considering the health and safety of the patient. The self-biased mentality in this case causes the severe problem of a patient's death. Therefore, such offence must be punishable as per the available legal guidelines. Moreover, the operating process of healthcare also needs to be changed to ensure the avoidance of such incidents in future.
Vulnerable people and groups are other aspects associated with the case of Mr. George. In this case, the professor protects his own interest through unethical actions rather than the actual actions that need to be considered. As per the study of Coleman et al. (2022), healthcare professionals must serve community interests rather than their own to match the nationalised treatment standards. Hence, considering this legal aspect also the professor is solely liable for the situation of Mr. George.
By analysing all the aspects, it can be stated that the family members need to lodge complaints specifically against the professor rather than all individuals to get a better response. Apart from that, the healthcare authorities need to organize investigations into the professor and consider strict punishments for such actions. It will help to prevent such unwanted events in future and avoid any legal obstacles in the operations.
- The nurses conduct in this instance have a lot of potential legal ramifications.
The problem of permission comes up first. Mr. George obviously did not provide informed permission before his procedure. This is a potential violation of his legal rights, which might result in a lawsuit for compensation.
The second problem is the CT scan. Whether or if Mr. George gave his permission for this surgery is unclear. If he didn't, the hospital may be in violation of federal law for executing an intrusive surgery without permission.
The urinary catheter is a problem, which brings us to point number three. Evidently, the nurse in question lacked the skills essential to perform a proper catheter insertion. The resulting anguish was so severe that it ultimately proved fatal for Mr. George. There is a possibility that the hospital may be held responsible for any damages that occur because of their carelessness.
The surgeon's actions are a problem, which brings us to our fourth point. The surgeon's behaviour toward the nurse constituted bullying and harassment, given his hostile and insulting tone. The nurse may file a lawsuit as a result of this.
Mr. George's passing is a last concern. This happened because the surgeon and hospital workers were careless. The hospital and the doctor might be held liable for Mr. George's family's suffering.
Conclusion
In this instance, the nurses' actions have far-reaching ramifications that may be pursued via the judicial system. To start, there is the problem of permission requests. According to all parties concerned, Mr. George did not provide authorization for the procedure that was performed on him. As a result of this infringement of his legal rights, he is entitled to monetary compensation. The second issue is a fault with the completed CT scan. Unknown is Mr. George's level of collaboration with this operation. If he hadn't given his consent, the hospital may face legal implications for performing an invasive procedure on a patient without his consent. In the third situation, the urinary catheter represents a major concern. Clearly, the nurse lacked the required expertise to insert the catheter into the patient. Mr. George passed away as a result of his trauma. The hospital may be held accountable for negligent treatment given the circumstances. Fourthly, the surgeon's behaviour is unsettling. The surgeon's behaviour toward the nurse, which included being rude and disrespectful, might be seen as an attempt to intimidate or harass the nurse. A nurse in this situation may choose to file a lawsuit against the medical institution for compensation. The final issue is Mr. George's passing. This happened due to the carelessness of the medical personnel and surgeon. The family of Mr. George may file a lawsuit against the hospital and the doctor for compensation.
References
.png)
.png)
PBHL20008 Engaging with Cross-Cultural Communities Assignment Sample
The assessment task for this unit is a reflective essay. Each student will write a reflective essay based on his or her experience of engaging with a cross-cultural community. Student can use example from their previous or current experience of working with a community group and reflect on communication and cultural challenges they experience. Students should then discuss learning they achieved from this experience and how they will apply that knowledge to improve their current or future public health practice.
The reflective essay will be assessed on the following criteria.
- The essay shows evidence of understanding of cross-cultural community engagement: 25%
- Reflection demonstrates use of appropriate language, personal learning and change in practice: 25%
- Reflexivity in linking personal experience, practice examples and evidence: 25%
- All work is the student's own, all information is properly referenced, and essay is written according to academic convention: 25%
- Students must achieve 50% in this assessment to pass the unit.
Solution
Introduction
The reflective assessment for assignment help will describe the personal up-liftment from the cross-cultural involvement with the indigenous groups. I will mention how the different communication obstacles would explore the opportunities so that the health care values and practices in Australia will be developed professionally.
Discussion
During the last summer in Adelaide, I participated in the international summer camp. This was the confluence of all the communities across different indigenous cultures in and beyond Australia (Lin et al., 2019). Amidst the sea of human heads, I found the people of Strait Islander interesting. I did works with the aboriginal community to get a taste of indigenous history. I was inspired in setting up cultural links with them getting past all the cultural constraints. The abundance of religious and cultural diversities supports the root of the culture. The intensive engagement with the different perspectives inculcates a renewed sense of cultural consciousness in me. They shared with me how they came into being, how they pass the present moments, and their future agendas. I felt a certain pride connecting to the home culture and knowing the minute details. It can be seen and felt how the communities share a warm bond trying to navigate the tricky corridors of life. They have a deep reverence for traditional values and community standards (Usher et al., 2021). The community prioritises authenticity, sincerity, and passionate deliverance. The rich cultures and beliefs are attuned to sustainable principles and value creation. I learned that the community people
Cultural and communication challenges were there that put me unease to accomplish the cultural mission objectives. I could not communicate properly and always hesitated in letting my thoughts unfold. I apprehended if the missions of the workshop would be successful. Some pervasive risks and challenges predominantly afflicted the emotional and social well-being of the islanders. Ethnocentrism struck me as the key barrier through which we get partial regarding the lens we look at the dimensions of the cultures. When these perspectives turned into prejudices a blind beliefs, the problems got worsened (Tynan et al., 2020). There was also a widened gap between their cultures and mine; anyhow, I tried to be in their shoes and perceived the communicational impediments. Along with that, comes the traditional tag of stereotyping which is also harmful to cultural cohesion and productivity. I was moved by the psychological barriers that amounted to the fact that widespread loss and grief have been part of the culture and I discovered the unresolved trauma therein. The lack of connection to the enlightened world led to their ignorance of health issues and the determinants of redressal (Yashadhana et al., 2020). The community governance is strong yet they have vulnerabilities to the various life-threatening dangers and losses. The indigenous community loves to pass on their cultural heritage and traditions but the sense of rootedness and belonging is overshadowed by the presence of negative factors. At some points, I felt that the practices in the system could have been more flexible to cope with the modern progression. Racial discrimination was something that entrenched its roots in the pristine soil. Moreover, the linguistic barriers were dominant that aggravated the communicational disputes. In addition, the geographical distance was much more than what I had previously idea and thought. The cultural disparateness added to the miscommunication, flawed mindsets, norms, and gestures (Moodie et al., 2021). Studying unfamiliar cultures and languages was the toughest part of working with the community and being exposed to cultural setbacks.
Personal experience is one of the best parts of the human life. I shook hands with some aboriginals and they considered it disrespectful. The respect for the community bonding was something they considered praiseworthy and I had lessons on the community rituals and customs. I had gathered lessons for them about the aboriginal arts and the ornamental designs on the physique are something they carry as a token of cultural heritage. The cultural baggage was abandoned and I took interest in the basketry and their values of social organisation (Russell-Smith et al., 2021). I learned the protocols and customs of the indigenous individuals and the overall well-being of the community people. IKSPS has been absorbed by me in harbouring the genuine feeling for the system and community values. I have understood that culture is the most symbolic asset for the community who are engaged in the making of history and traditions. All aspects of life have been permeated by cultural lineage and local diversity. I have gained another important knowledge regarding the conservation of policies and wealth. Other participants from abroad also came in contact with the different attributes and therefore, the culture was replete with all the resources and native pride. The cross-cultural symbolism made it easier to contact the different cultures and the people.
In the future, I shall apply the learning in public health practice and implement the protocols to remove the risks that can be harmful to the aboriginals. They are believed to have been the sufferers of chronic diseases like pneumonia, heart disease depression, and many more. Therefore, I will be sincere in offering value-based care to the patients. I have decided to apply the value theory proposed by Walras, Jevons, and Menger. The encompassing theory takes into consideration all the moral practices, ethics and responsible duties to safeguard the lives of the people. Many aboriginals are victims of paranoia, stress, and distressing mental condition due to the loss of lands, and separation from family and children. Many of them are suffering from identity issues and cultural estrangement that gave rise to health problems and many more additional health crises. Incarceration, substance misuse, and violence can be seen among the cultures that decreased the values and increased panic. I will teach them about the indication of environmental degradation, industrial activities as well as many more on health and comprehensive development. If the illicit abuses of drugs and alcohol can be stopped, better immunisation practices could be developed (Yashadhana et al., 2020). I feel that the indigenous community must be sincere in protecting their rights, and stopping their involvement in the criminal system, and better health practices can be created.
Conclusion
This is clear from the above discussion that a deeper connection with the culture can empower the historical and culturally conscious self. I have gained deep learning from the involvement at a deeper level and this is beneficial for protecting the health care sector.
Reference List
.png)
SPS201 Alcohol and Other Drugs Essay 1 Sample
Assignment Brief
a) Description
This assessment requires analysis on three foundational areas of learning –
1. Understanding of addiction
2. The Cycle of Addiction
3. Evidence based models (choose one evidence-based model only)
b) Format
To be successful in this assessment you must address all three areas. You are required to clearly demonstrate your understanding of what addiction is, in terms of your what you have learnt, how the cycle of addiction impacts as well as giving a very clear understanding of one evidence-based model.
This assessment serves as a preparatory guide to the learning that students are expected to acquire and develops the research and analysis skills required to complete subsequent assessments. Your assessment must be submitted through Turnitin and must adhere to the College’s academic integrity and authorship requirements. The questions and instructions contained in the file will be available three weeks before the due date.
Note Research literature
Your essay must be based on a review of the literature and should include at least five primary academic references, ie peer-reviewed (scholarly) journal articles or book chapters. Do not rely upon non-academic and other web-based secondary references as these do not constitute academic references for the purpose of your assignment, which if relied upon for theoretical support, may mean you have NOT met the requirements of the assessment.
Referencing
You must use APA 7 referencing.
Table of references: You must include a Table of references section in your essay and acknowledge any sources that you use, including all web-based sources.
Structure of essay
As the assignment conveniently provides the three foundational areas to be addressed, there is a lot of sense to use them as headings, as they form the basis of assessment criteria. If there are identifiable questions or sub-issues within each heading, then it may be a good strategy to also include these as sub-headings under each heading.
Solution
Introduction
The nature of addiction is examined in this essay within the context of neurobiological disease and a learned behaviour due to sociocognitive factors. Therefore, using the existing social learning model this study aims to uncover the different dimensions of addiction such as compulsive use, loss of control as well as continued use despite negative consequences. Further, the essay evaluates downstream and upstream processes of the substance dependence that involves questions like withdrawal, relapse, and detoxification to demonstrate the problems that people encounter in their recovery. Thus, this work aims at presenting information concerning effective strategies in the treatment of addiction with regard to the psychological and social spheres.
Understanding of Addiction
Figure 1: Addiction as a brain disease
Source: (Surgeon General, 2016)
The diagram shows that there are identified changes in areas that are unidentifiable in the brain, and these areas are generally related to different stages of addiction. Giving examples it can be added that there is a concept of three stages, preoccupation or anticipation, binge or intoxication and withdrawal or negative affect and associated specific parts of the brain are described (Surgeon General, 2016). Addiction is widely accepted and defined as a neuropsychological disorder with genetically determined behavioral deregulation, impaired control over drug and other addictive behaviors, and negative life consequences (Siomek-Gorecka et al., 2021). This disease conception of addiction is rooted in knowledge that continued use of substances or participation in addictive activities can alter the brain structure especially in areas like, reward, motivation, and memory. The brain circuits which seem to become involved when a person has an impulse to stop participating in an addictive activity, get affected and results to the inability of individuals to cease indulging themselves in the addictive process even when they want to.
The simplest definition of addiction is a psychological and physical reliance on an object or an activity. It therefore leads to craving and reward cycle which in one way or the other has negative effects on the user, the surrounding society and physical wellbeing (Wiers, and Verschure, 2021). Addiction can be explained through certain feature: Compulsive use, the need to perform the addictive behavior despite the adverse effects. On the other hand there is an impulsivity issue when persons lose control over their actions or decisions, despite being able to comprehend the consequences of their actions. The last stage is continued use, where the person continues with the behaviour despite adverse consequences, and often tend to minimize them in their lives for the assignment helpline.
The Cycle of Addiction
The addiction cycle is a cycle of dependency which include phases such as withdrawal, relapse and detoxification all of which cause dependency. Detoxification is characterized by the outward withdrawal from the addictive behavior and one notices adverse emotions or physical sensations, which are normally associated with the addictive substance. Different substances or behaviors will cause different kinds of withdrawal symptoms, but they all prompt the person to engage in the behavior again in order to escape the physical or emotional discomfort associated with withdrawal (American addiction centers, 2019).
Relapse as the crucial stage in the cycle of addiction implies returning once again to the process of using a substance as well as coming back to those situations when controlling impulses is impossible because of the urge’s extremity. Hence it can be added that it is a common and challenging aspect of recovery that mainly reflects on the chronic nature of addiction (Guenzel and McChargue, 2023). Detoxification, on the other hand, entails clearing the body of substances that one is addicted to and most often patients undergo it under the close supervision of the doctor because withdrawal can come with its side effects. Detox is used, as a rule, at the early stage of therapy; its goal is to eliminate physical dependence on the substance and finalization of withdrawal symptoms before starting counselling and therapy.
Evidence Based Models: The Social Learning Model
The social learning model is an empirically supported theoretical orientation for understanding substance dependence in which learned behaviours, environmental stimuli and interpretations and meditational processes are central. This model propounds that dependence behaviour including alcoholism results from observational learning and reinforcement. The social learning model does not consider addiction a singular, stable, and singular state of affairs, but certainly provides a dimensional form encompassing a constellation of behaviors and implications that can affect individuals’ different sides with different degrees of addiction dependent on their social environment, choice, and perception (Smith, 2021).
The social learning theory revolves around the fact that addiction is learned through the late recoils which are usually picked from other people in the society, peers or even family members, media personalities. The external environment hence involves what people see around them in form of behaviors over substance use or other forms of addictions where they may be tempted to perceive these actions as ways of handling stress or some pressures. These behaviours remain learned because when behaviour is associated with perceived rewards such as relief from anxious states, social acceptance or pleasure. Because of this reinforcement, addiction-related behavior becomes strengthened and will most likely lead to habitual actions (Brady et al., 2021).
Cognitive processes also have a role in social learning model since people’s perception about the substance or behaviors can either lead them to engage in addiction. For example, if the learners think that alcohol will help them to overcome social phobia, they will be most likely to take alcohol in social events. Additionally perceiving the negative consequences downplaying the risks or overestimating control over usage, can maintain addiction behaviours. These cognitive processes, along with those learned behavioral responses, form the cycle that then perpetuates addiction.
Therefore, the social learning model supports the forms of treatment that tackle the behavioral as well as the cognitive parts; they may use treatments such as Cognitive-Behavioral Therapy (CBT). Offering guidance on identifying and directly confronting addictive beliefs, replacing negative behaviors with helpful ones, the model offers a clear structure for establishing long-term recovery, in a way expressing the conclusion that addiction is not exclusively the result of a person’s inherited traits and tendencies, but also a stably developed response to learned stimuli (Smith, 2021).
Conclusion
Hence it can be concluded that addiction includes biological, psychological and social determinants. The essay researched that addiction is not a simple issue but is witnessed through the cycle of dependency and learning that supports it. The social learning model offers an insight into the broaden scope of behavior and cognition influencing addiction and adding to its maintenance. In addition to that it can be added that implementing effective interventions is essential as it targets both behavioral and cognitive aspects fostering long term recovery through different strategies such as cognitive therapy. Hence addressing such addiction from implementing multidimensional perspective can help in developing better and efficient comprehensive and impactful support systems for those affected by drug addictions.
References
.png)



.png)
~5.png)
.png)
~1.png)



















































.png)






